Transaction enrollment
Transaction enrollment is the process of registering a provider to exchange specific healthcare transactions with a payer. It involves submitting information about the provider, including their name, tax ID, NPI, billing address, and contact information.
Electronic Remittance Advice (ERAs): Don't enroll until you're ready to switch to Stedi. Once you enroll, all ERAs from that payer will come through Stedi exclusively. You'll no longer receive ERAs from that payer through your previous clearinghouse.
Do I need to enroll my provider?
For 835 ERAs, always yes. For other transactions, it depends on the payer.
Check the Payer Network or use the Payers API to determine whether your payers require enrollment for the transaction types you want to send and receive. Each transaction type is marked as either:
- Supported, enrollment not required
- Supported, enrollment required
- Not supported
For example, the following payer record shows that Blue Cross Blue Shield of North Carolina requires enrollments for 835 ERAs, as indicated in the transactionSupport.claimPayment property.
{
"stediId": "UPICO",
"displayName": "Blue Cross Blue Shield of North Carolina",
"primaryPayerId": "BCSNC",
"transactionSupport": {
"eligibilityCheck": "SUPPORTED",
"claimStatus": "SUPPORTED",
"claimSubmission": "SUPPORTED",
"claimPayment": "ENROLLMENT_REQUIRED",
"dentalClaimSubmission": "SUPPORTED",
"professionalClaimSubmission": "SUPPORTED",
"institutionalClaimSubmission": "SUPPORTED",
"coordinationOfBenefits": "SUPPORTED",
"unsolicitedClaimAttachment": "NOT_SUPPORTED"
}
// truncated for brevity
}If enrollment for a supported transaction type is:
- Not required: The provider can start exchanging transactions through Stedi right away. They'll include their information (like their NPI) in transactions as needed.
- Required: The provider must complete transaction enrollment before they can start exchanging those transactions through Stedi. Note that ERA enrollment is exclusive to one clearinghouse. Switching a provider to Stedi stops ERA delivery through the previous clearinghouse.
How long does enrollment take?
Most enrollments are completed within 24 - 48 hours. However, some payers may take up to 30 days, depending on their internal processes and requirements.
Check out FAQ for answers to other common questions about transaction enrollment.
Enrollment process
Stedi handles the entire enrollment process for you, including submitting the required information to the payer and monitoring the status of the enrollment.
Here's how it works:
The provider record includes the information required to enroll the provider with payers, including the provider's name, tax ID, NPI, and contact information.
You can create enrollment requests individually through the Stedi portal, in bulk through CSV import, or programmatically through the API. Stedi gets alerted about new enrollment requests once they're in STEDI_ACTION_REQUIRED status.
For each provider, you'll create one enrollment request per transaction type. For example, you would create three separate requests to enroll a provider for 837P professional claims, 270 real-time eligibility checks, and 835 ERAs.
When we begin the enrollment process with the payer, we'll set the enrollment status to PROVISIONING. We'll reach out to you in your dedicated Slack or Teams channel with resources and to answer any follow-up questions.
For some payers, such as those with one-click enrollment, Stedi can complete the entire enrollment process for you. We sign enrollment PDF forms on your behalf, when possible, to speed up the process and eliminate extra work for your team.
If payers require additional steps from providers as part of their standard enrollment process, Stedi sets the enrollment status to PROVIDER_ACTION_REQUIRED and adds a task to the enrollment request with clear instructions. The enrollment process continues once the required tasks are completed.
You can check which payers require additional steps on our Transaction Enrollments Hub.
Once the enrollment is approved, the enrollment status is set to LIVE, and the provider can start exchanging the enrolled transactions with the payer.
Enrollment statuses
An enrollment request can have one of the following statuses:
DRAFT: You are still editing the record and it has not been submitted to Stedi.STEDI_ACTION_REQUIRED: You have submitted the enrollment and it is ready for Stedi to begin processing.PROVIDER_ACTION_REQUIRED: The enrollment requires action from the healthcare provider to proceed, such as providing additional documentation. Stedi will add a note to your enrollment request with clear instructions.PROVISIONING: Stedi has begun the process of completing the enrollment with the payer.LIVE: The enrollment process is complete, and the specified provider can begin exchanging the listed transaction types with the payer.REJECTED: The payer rejected the enrollment. Common reasons for rejection include incorrect details in the request and that the provider is not credentialed with the payer. Customer support will contact you with reasons for rejection and next steps.CANCELED: The enrollment has been terminated per customer or provider request. You can only cancel enrollments that are inDRAFT,STEDI_ACTION_REQUIRED, orPROVIDER_ACTION_REQUIREDstatus.
One-click enrollment
We offer one-click enrollment for eligible payers. Once you submit the enrollment request, Stedi handles the entire process without any additional action from you. These payers don't require any signatures or documentation other than what is included in the enrollment request.
You can determine whether a payer is eligible for one-click enrollment by:
- Checking the Payer Network. Click a payer's name to view its details. Stedi lists the Type as One-click for transaction types that support one-click enrollment.
- Calling the Payers API. The
enrollment.transactionEnrollmentProcesses.{transactionType}.typeproperty is set toONE_CLICKfor transaction types that support one-click enrollment.
Rejected enrollments
In rare cases, the enrollment status might be set to REJECTED if the payer denies the enrollment request. Rejection can happen for many reasons, but the most common are:
- The provider isn't credentialed with the payer. If a payer rejects your transaction enrollment request with a message indicating the provider is "not on file" or "not recognized," it likely means the provider hasn't completed credentialing and payer enrollment with that payer. Visit Credentialing and enrollment to learn more.
- There was incorrect data in the enrollment submission.
If an enrollment is rejected, Stedi puts a note on the enrollment request explaining the reason and how to resolve it. You can review the note through the UI or API and contact Stedi support in Slack or Teams with any additional questions.
Create enrollment requests
An enrollment request includes the provider record, the transaction type you want to enroll, the payer you want to enroll with, and a designated contact that the payer can communicate with about the enrollment. All requests go through the same high-level enrollment process once submitted.
Developers can create enrollment requests individually, through bulk CSV import, or through the API.
Individual UI submission
Creating individual enrollment requests through the Stedi portal involves two steps:
- Create a provider record: Visit the Providers page and click New provider. Enter the provider's information. Review our guidance on provider contact information to ensure updates go to the correct location.
- Create an enrollment request: Visit the Enrollments page and click New enrollment. Select the provider, transaction type, payer, and contact email. Requests are automatically submitted to Stedi upon creation.
Bulk CSV import
To create enrollment requests, go to the Bulk imports page and click New bulk import.
The upload page contains detailed instructions for formatting the CSV file. Once you upload the file, Stedi checks for errors and flags any rows that require adjustments. You can either fix the errors and re-upload the CSV file or click Continue anyway to proceed with importing valid rows.
Stedi automatically does the following when importing enrollment requests from a CSV file:
- Creates provider records as needed. Stedi creates a new provider record for each unique combination of NPI and tax ID in the CSV file. For example, these two providers would be created as separate records even though they have the same name and NPI:
John Doe, NPI: 1999999984, Tax ID: 987654321John Doe, NPI: 1999999984, Tax ID: 123456789When a row in your CSV file contains an NPI and tax ID that match an existing provider record, Stedi overwrites the existing provider record with the information in the CSV file. Any changes (such as updated address or contact information) aren't automatically applied to existing enrollment requests for that provider, only to requests created after Stedi updated the record.
- Creates and submits enrollment requests. You can check the status of each request through the Enrollments page once the import is complete.
- Removes duplicate rows to prevent duplicate requests.
- Checks for errors. Stedi imports valid rows and skips any that contain errors. For example, if a row contains an invalid NPI, Stedi skips that row and imports the rest of the file.
Import status report
After importing, you can download a report that shows the status of each row in the CSV file. For example, duplicate rows are marked as Duplicate: Enrollment already exists in the result column.
Rows with errors display a clear inline error message to help you quickly make the necessary adjustments. You can fix rows with errors and re-upload the CSV file as many times as needed until all imports are successful.
API submission
Creating enrollment requests programmatically through Stedi APIs involves two steps:
- Create a provider record: Call the Create Provider endpoint.
- Create an enrollment request: Call the Create Enrollment endpoint. You can create enrollment requests in
DRAFTstatus first and change the status toSUBMITTEDlater when you're ready to submit them to Stedi. Stedi won't process the enrollment until it is inSUBMITTEDstatus.
Enrollment contact information
When you submit an enrollment requests, you'll need to provide two types of contact information. It's important to understand the difference between them.
Provider contact
This is where the payer will send communications about the enrollment, if needed.
- The name and address should match exactly what the payer has on file for the provider. Some payers reject enrollment requests with addresses that don't match their records.
- However, you may want to set the phone number or email to a different contact - for example, a credentialing or general inbox - to ensure payer communications go to the right place.
- If you're enrolling a group practice, select a single administrative entity as the contact - don't use individual provider emails.
Submitter email
This is the email address where Stedi will send updates about the enrollment. We'll use it to notify you when there are next steps and send updates on the enrollment's status.
This is called the userEmail property in the Stedi API, the user_email column in the CSV file for bulk imports, and the Person for Stedi to contact in the UI form.
This email address can be different from the contact information you provided in the provider record. Set it to wherever you want to receive Stedi's communications about the enrollment.
Manage tasks
Tasks are actions that either the provider or Stedi need to complete to move the enrollment process forward. Tasks can include:
- Providing additional documentation or signatures.
- Completing payer-specific requirements.
- Reviewing and confirming details.
When there's a new task that requires the provider to take action, Stedi adds a task to the enrollment request with instructions and sets the enrollment status to Provider Action Required. The email address listed as the Person for Stedi to contact will also receive a notification that there's a new task to complete.
You can review and manage tasks at the top of the enrollment request's details page in the Stedi portal. Once you've taken the required action, check the box next to the task to mark it as complete. Stedi is automatically notified when you complete a task, and the enrollment process continues.
Manage documents
Some payers require additional documents to complete the enrollment process, such as:
- Signed enrollment forms
- A practice's W-9 tax form
- A voided check
We'll send you a notification when enrollment requests require additional documentation. You can download the required forms and upload completed documents to Stedi. Only PDF files are supported.
API
You can use the following API endpoints to manage enrollment documents programmatically:
- Upload Enrollment Document: Get a pre-signed URL to upload a PDF document related to a specific enrollment request.
- Download Enrollment Document: Get a pre-signed URL to download a specific PDF document related to an enrollment request.
- Delete Enrollment Document: Delete a specific PDF document related to an enrollment request.
Enrollments UI
To upload PDF documents in the Stedi portal:
- Go to the Enrollments page and click the enrollment request that requires documentation.
- Scroll to the Documents section at the bottom of the page.
- Click Upload new document and choose the PDF file you want to upload.
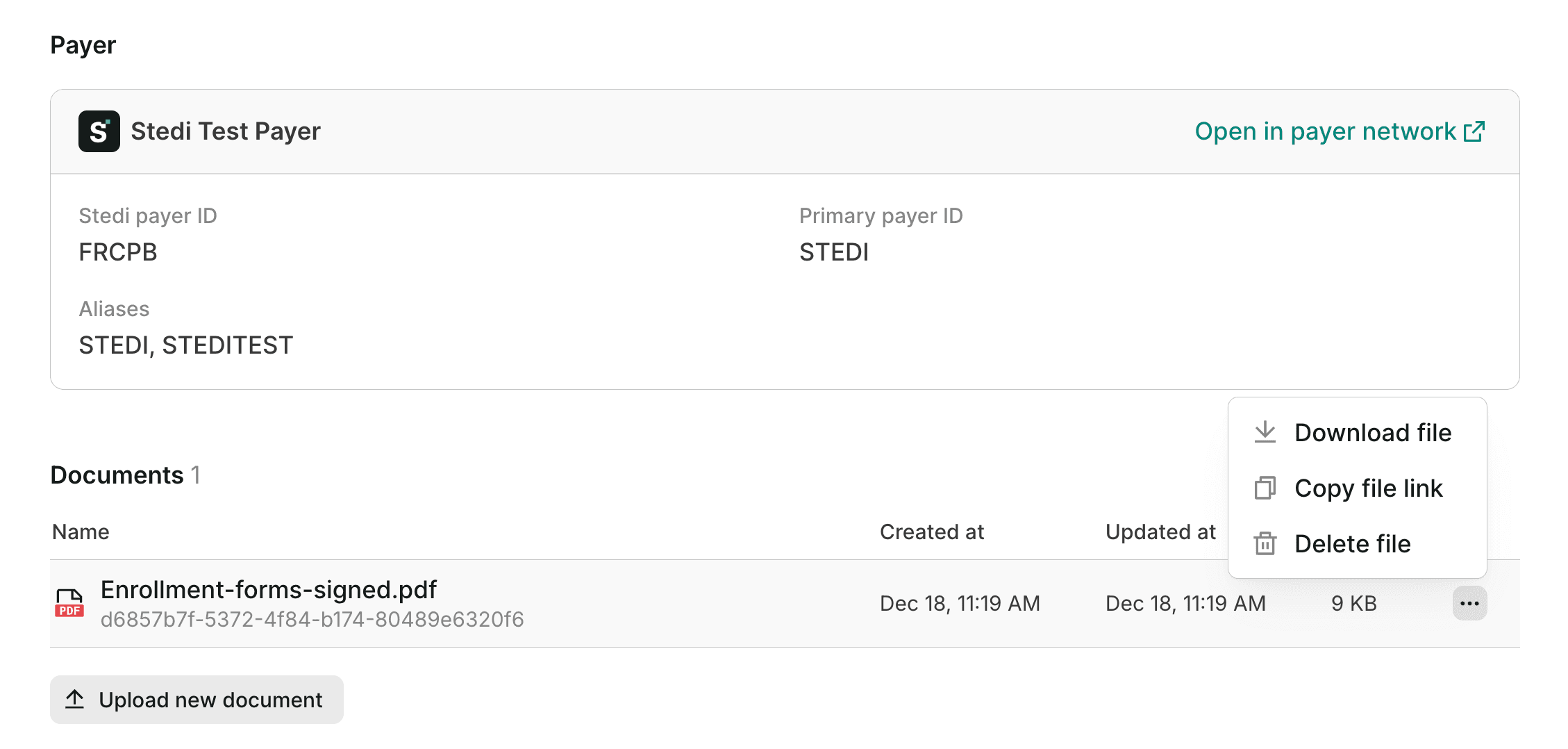
Uploaded documents are listed in the Documents section. Click any document to view it in your web browser. You can also click ... (ellipses) to the right of the document to:
- Download the original PDF file.
- Copy a secure link to view the file, which you can share with any member of your Stedi account.
- Delete the file, if necessary.
Review enrollment details
You can track the status of your transaction enrollment requests from the Enrollments page in your account.
Click an enrollment request to view its details, including:
- The provider and payer associated with the enrollment.
- The transaction types included in the enrollment.
- The current status of the enrollment.
- Any notes or instructions from Stedi or the payer.
- The history of status changes and actions taken on the enrollment.
- Enrollment documents, such as signed PDF forms.
Alternatively, you can retrieve information about enrollment requests through the List Enrollments endpoint.
Cancel enrollments
You can only cancel enrollment requests that are in DRAFT, STEDI_ACTION_REQUIRED, or PROVIDER_ACTION_REQUIRED status. Reach out to Stedi support in Slack or Teams to cancel. Once an enrollment is canceled, Stedi sets its status to CANCELED and stops the enrollment process with the payer.
We can't cancel enrollments that are in PROVISIONING or LIVE status. Once an enrollment is in one of these statuses, the only way to stop 835 ERAs from coming to Stedi is to submit an enrollment through another clearinghouse.
Notification emails
Stedi sends a notification email once per hour with a summary of enrollment request status changes. The email includes a link to each enrollment request where you can review notes, instructions, and other details.
Email notifications are sent to the address designated as the Person for Stedi to contact about the enrollment. This is typically the email associated with the Stedi account that created the enrollment request, and it may differ from the provider's designated contact.
If you aren't receiving notification emails as expected, contact Stedi support in Slack or Teams.
CMS auto-enrollment
The Centers for Medicare and Medicaid Services (CMS) is one of the few payers that requires enrollment for eligibility checks.
Eligibility checks to CMS fail with AAA error 41 when a provider isn't properly enrolled. In these cases, Stedi automatically submits the required transaction enrollment request. CMS usually processes these enrollments within 24-48 hours.
Please note:
- If the provider's NPI isn't active in the National Plan & Provider Enumeration System (NPPES), Stedi won't automatically create the enrollment for the NPI. The provider will need to apply directly with CMS to be added to the registry.
- If the provider's NPI isn't active in PECOS, the system CMS uses to manage active Medicare providers, the transaction enrollment request will be rejected and set to
REJECTEDstatus. If that happens, we'll send you instructions explaining how to resolve the issue.
Enrollments hub
Our network and enrollment operations team knows the nuances of each payer’s enrollment requirements and maintains a public repository of payers that require additional steps through our Transaction Enrollments Hub.
Practices and facilities with multiple providers or locations
Some healthcare organizations operate multiple facilities or practices under a shared structure. This is common in hospital systems, clinic networks, or large medical groups where multiple service locations operate under the same billing entity.
Transaction enrollment requires the billing provider's tax ID and NPI that you plan to use in claims and Electronic Remittance Advice (ERAs). When the same group NPI and tax ID are used as the billing provider throughout the healthcare organization, you should:
- Create a single provider record with that NPI and the tax ID. You don't need to create provider records for individual rendering providers.
- Create enrollment requests with the billing provider record attached. You don't need to submit additional enrollment requests for individual rendering providers. Select a single administrative entity as the contact - don't include individual provider emails. This should be a credentialing or general inbox.
- Use the taxonomy code that matches the billing provider's credentials when submitting claims.
FAQ
Do I need to enroll through Stedi if I'm already enrolled through another clearinghouse?
Yes. Enrollment is specific to each clearinghouse. So if a payer requires enrollment, you will need to go through the enrollment process with Stedi to begin exchanging transactions through the Stedi clearinghouse.
What will happen to the ERAs I currently receive through a different clearinghouse?
ERAs can only be sent to a single clearinghouse. Once you enroll for ERAs through Stedi, all ERAs from that payer to the provider you enrolled will come through Stedi. The provider will no longer receive ERAs from that payer through your previous clearinghouse.
Does enrolling with Stedi cancel my enrollment with another clearinghouse?
For ERAs, yes. Once you enroll for ERAs through Stedi, the payer will stop sending ERAs to your previous clearinghouse.
For claims and other types of transactions, it depends on the payer. Some payers accept claims through multiple clearinghouses or direct connections. Customer support can help answer this question for your specific payers.
Can a provider be enrolled through multiple clearinghouses at the same time?
Yes, for claims and eligibility checks. Some payers allow providers to submit claims and eligibility checks through multiple clearinghouses. Customer support can help answer this question for your specific payers.
No, for ERAs. As soon as an ERA enrollment in Stedi is processed with the payer, you won't receive ERAs through your previous clearinghouse.
Can I send claims through Stedi without switching my ERA enrollments?
Yes, you can start sending claims through Stedi without enrolling for ERAs. The ERAs will still go to your current clearinghouse. In Stedi, you'll see the claim and the 277CA claim acknowledgment from the payer, but you won't see ERAs until you switch those enrollments to Stedi.
