Eligibility searches view
The eligibility searches view provides insight into your eligibility check pipeline and helps you identify, diagnose, and fix failed eligibility checks. For example, you can filter for all the eligibility checks that failed during a payer outage and retry once the payer is back online.
In the app, you can:
- Review every eligibility check you submit through the app or Stedi APIs.
- Search and filter historical eligibility checks by status, Payer ID, date, and error code.
- Edit and retry failed eligibility checks and review the details of each attempt. With the Stedi Agent, you can resolve common recoverable errors automatically with the same best practices our Support team uses for troubleshooting.
- Use the Debug view to systematically troubleshoot failed eligibility checks until you receive a successful response from the payer.
Example troubleshooting workflow
The following example shows how the eligibility searches view can help you track and resolve eligibility check failures:
You submit an eligibility check through Stedi's Eligibility Check API for Nick Smith. Stedi sends it to the payer and creates a new eligibility search record in the app containing the request details.
The payer returns an AAA
error code 75 -
Subscriber/Insured Not Found. The eligibility searches view shows that the
status for the new eligibility search is Failed.
You open the eligibility search, diagnose the error, correct the subscriber's first name to "Nicholas", and submit the updated eligibility check. Stedi stores the updated request as another entry in the existing eligibility search.
The payer returns a successful response showing active insurance coverage
for Nicholas Smith. The status of the Eligibility Search changes to
Active, and you can view the request and response details for both
iterations of the eligibility check - the original failure and the
successful retry - within the same eligibility search record.
Eligibility search
Stedi stores eligibility check requests in groups called eligibility searches.
When you submit an eligibility check through the app or API, Stedi creates a new eligibility search record. Every time you retry that eligibility check, Stedi stores the retry details within the existing eligibility search. This creates a clear timeline of troubleshooting efforts for failed requests.
Create
You can create a new eligibility search through the app or Stedi APIs.
- App: Go to the Eligibility searches view and click + New eligibility check.
- API: Use the Eligibility Check API to submit an eligibility check programmatically.
Once you submit the eligibility check, Stedi creates a new eligibility search in the app.
External Patient ID
You can optionally add a External Patient ID to the request. This should be a unique identifier for the patient in your system. Adding this identifier helps you identify eligibility checks for the same patient over time.
Filter
You can filter eligibility searches by the following criteria:
- Error code: By the AAA code returned by the payer. For example,
42errors indicate a connectivity issue. - Payer: By the Payer ID (62308) or business name (such as Cigna)
- Status: By Queued, Started, Failed, Inactive, and Active
- Date: A date range for when the initial eligibility check within an eligibility search was submitted. For example, a filter beginning on October 1st would only include eligibility searches with an initial submission on or after October 1st. It would not include an eligibility search with an initial submission on September 30th and a retry on October 1st.
- Provider NPI: By the National Provider Identifier (NPI) of the requesting provider.
Results are sorted by the date of the original eligibility check within the eligibility search, with the most recent listed first.
Statuses
The status of an eligibility search is determined by the most recent eligibility check in the record. For example, if the most recent iteration of a check failed, the status of the entire eligibility search is Failed, even if a previous version of the request succeeded.
An eligibility search can have one of the following statuses:
- Queued: Stedi placed the eligibility check in its internal queue and will send it to the payer when resources are available. This status is common when you schedule batch eligibility check refreshes through the API or perform large bulk retries that exceed your account's concurrency budget. You can typically expect the status to change to
Startedwithin a few seconds. - Started: Stedi sent your eligibility check to the payer and is waiting for a response.
- Failed: The payer returned an error code in the response. Review the error code and retry the eligibility check.
- Inactive: The payer's response doesn't contain an active eligibility and benefit type.
- Active: The payer's response contains an active eligibility and benefit type (codes 1-5). Visit Eligibility and benefit type codes for a complete list.
Get payer details with the Stedi Agent
The Stedi Agent is an AI assistant that can answer your questions about supported payers. To use it, you must be at least an Operator role within your Stedi account.
The Stedi Agent can help you:
- Determine the correct payer ID for supported payers
- Map your internal payer names to Stedi's supported payers
- Determine which payers require transaction enrollment
- Identify which payers support medical, dental, or both use cases
- Get help with other payer-related questions
To start chatting with the Stedi Agent:
- Go to the Chats page in the Stedi portal.
- Click New chat and select Payer Finder.
- Type your question in the chat window and press Enter. For example, you could ask "What is the payer ID for Aetna?" or "Does Cigna support dental use cases?" You can also ask more complex questions, like "Which payers support dental use cases and require transaction enrollment?" Talk to Stedi Agent like you would a human support agent.
- Ask follow-up questions as needed. You can ask multiple questions about different payers in the same chat.
The Stedi Agent will respond to your questions and display its answers in the chat window.
Review chat history
You can review a list of all past chats with Stedi Agent on the Chats page. Click any chat to open it and review the conversation. You can restart any previous chat by sending a new message. Note that this page also contains the agent's eligibility recovery attempts, which are read only.
Review eligibility check errors
The Eligibility check errors page shows a list of recent eligibility check AAA error codes. These are errors the payer returns when they reject your eligibility request. They specify the reasons for rejection and any recommended follow-up actions.
To go to this page, open the Eligibility menu in the navigation bar and select Errors.
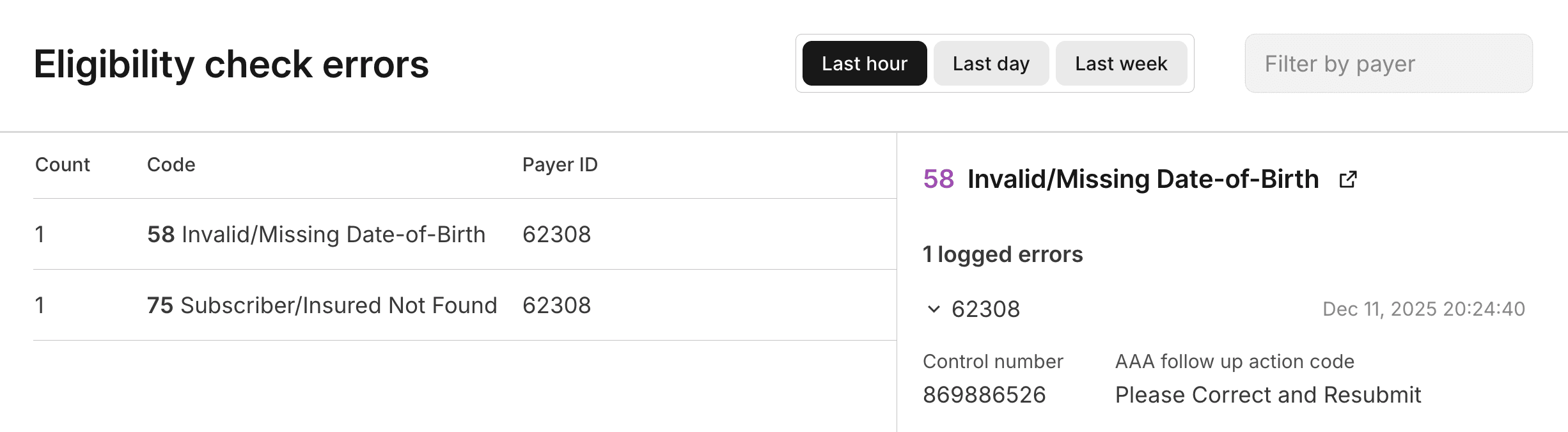
The errors are grouped by error code, and you can filter the list by Payer ID. You can look up any payer's ID in the Payer Network. Click on an error code to review a list of all the instances of that error.
This page helps you identify patterns in eligibility check failures. For example, if you see a large number of errors with code 75 (Subscriber/Insured Not Found) for a specific payer, you might want to investigate whether there are common issues with the patient data being submitted to that payer.
Visit Payer AAA errors for a complete list of AAA errors and their possible causes and resolutions.
Retry failed eligibility checks
When an eligibility check fails, you can edit the request details and resubmit it until you get a successful response. You can either retry the entire eligibility search (the latest iteration of the eligibility check) or select a specific iteration to retry.
There are three ways to retry a failed eligibility check: using the Stedi Agent, manually resubmitting the request, or using Debug view.
Retry with the Stedi Agent
You can use the Stedi Agent to troubleshoot and resolve common recoverable eligibility check errors automatically. To use it, you must be at least an Operator role within your Stedi account.
To resolve an eligibility check failure with the Stedi Agent:
- Go to the Eligibility searches view.
- Click Resolve with Stedi Agent next to an eligibility search. This is button is only available next to eligibility searches with common recoverable errors.
- The Stedi Agent opens a side panel in Debug view.
- The Stedi Agent analyzes the eligibility request and works through best practice recovery strategies based on the error type. For example, if the payer returned an error code
75(Subscriber/Insured Not Found), the agent may try different combinations of patient data or adjust the name format to find a match in the payer's system.
Each time the agent retries the eligibility check, it stores the new request in the same eligibility search record and it shows up in Debug view in real time. This allows you to see the history of attempts and the progression of the agent's troubleshooting efforts.
The agent only accesses data from the eligibility search it's working on. It can't access data from other searches, customers, or systems.
You can review past recovery attempts with Stedi Agent from the Chats page. These attempts are read only - you won't be able to send chat messages to the agent.
Manually edit and retry
To manually resubmit an eligibility check:
- Go to the Eligibility searches view.
- Click the eligibility search you want to troubleshoot to view its details.
- Click Actions > Edit and retry.
- Update the request details as needed, and click Submit.
You'll know the retry was successful when the status of the eligibility search is either Active or Inactive. If the status of the eligibility search is still Failed, you may want to try resolving in Debug view or using the Stedi Agent, if available.
Iterate in Debug view
Debug view is a workspace where you can systematically troubleshoot failed eligibility checks until you receive a successful response from the payer. For example, first you might try swapping the patient's nickname (Dave) for their full name (David) to see if that returns benefits information. In the next iteration, you might try submitting the request with a different service type code or dropping the date of birth.
Debug view shows all past iterations of the eligibility check and highlights the differences between each new version of the request. You can also draft and submit new requests directly from this page. This format helps you understand what you've already tried and quickly iterate on failed requests.
To troubleshoot eligibility checks in Debug view:
- Go to the Eligibility searches view.
- Click the eligibility search you want to troubleshoot to view its details.
- Click Actions > Debug to enter Debug view.
- Click + Add draft to create a new draft request. Stedi pre-populates the draft with the details from the most recent eligibility check in the search.
- Update the draft request as needed. Use the Edit columns list to show or hide specific fields in the request.
- Click the green arrow when you're ready to submit the updated eligibility check draft.
Stedi runs the check and moves it to the list of Past checks. Stedi highlights the differences between it and other past checks so you can see a clear record of your troubleshooting efforts. You can repeat this process as many times as needed to get a successful response.
Link to specific eligibility checks
Stedi assigns a globally unique identifier to each eligibility check, formatted as ec_<UUID>. For example: ec_f81d4fae-7dec-11d0-a765-00a0c91e6b12.
The unique eligibility check ID is returned in the following locations:
- SOAP Eligibility Check endpoint:
stedi-idheader in the HTTP response - JSON and Raw X12 Eligibility Check endpoints
idproperty in the JSON response - Poll Batch Checks endpoint:
items.idproperty in the JSON response - Retrieve Batch Check Statuses endpoint:
items[].additionalInfo.eligibility.idproperty in the JSON response
You can use the eligibility check ID to link directly to a specific eligibility check's results in the Stedi portal. The format for direct portal links is: https://portal.stedi.com/app/healthcare/eligibility/{search-id}/inspect/{check-id}, where {search-id} is the eligibility search ID and {check-id} is the unique Stedi-assigned eligibility check ID.
You can find the eligibility search ID at the top of an eligibility search's details page. Visit the Eligibility searches view for a list of your eligibility searches.
Stedi Agent usage notes
Please note:
- The Stedi Agent is available on all paid Stedi plans at no additional cost beyond those for related API calls.
- The agent is assistive. Outputs can be incorrect or incomplete. Verify all responses before taking any action based on them.
- You are responsible for any actions you instruct or authorize the AI service to take, including generating billable requests on your behalf.
- Your chats with the Stedi Agent aren't private - they're visible to anyone with access to your Stedi account.