Eligibility troubleshooting
A list of potential errors and possible resolutions when submitting 270/271 eligibility checks.
Review eligibility check errors
The Eligibility check errors page shows a list of recent eligibility check AAA error codes. These are errors the payer returns when they reject your eligibility request. They specify the reasons for rejection and any recommended follow-up actions.
To go to this page, open the Eligibility menu in the navigation bar and select Errors.
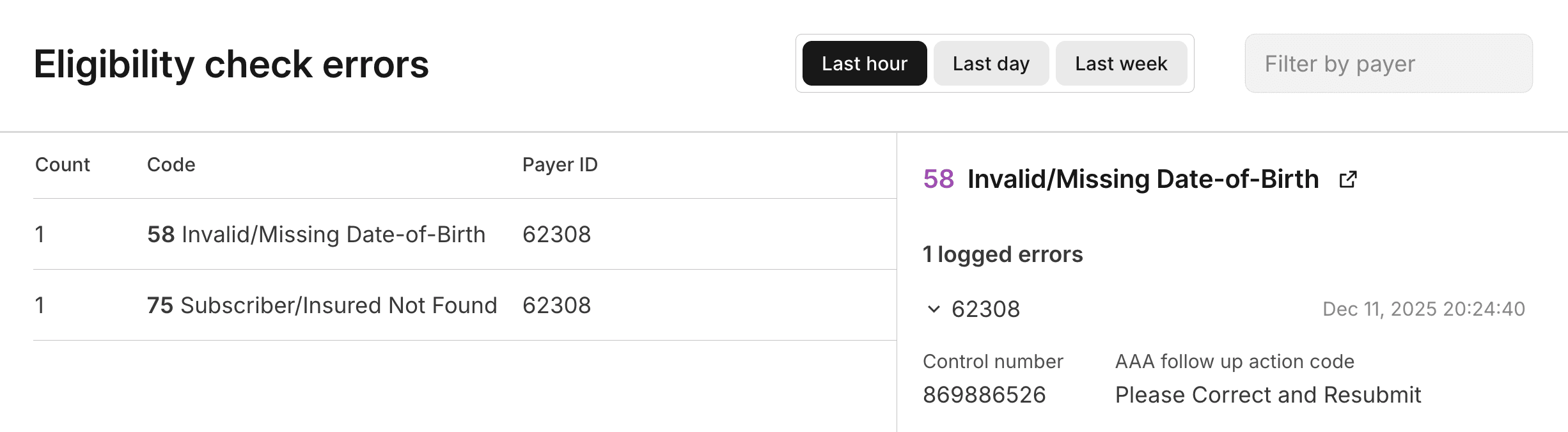
The errors are grouped by error code, and you can filter the list by Payer ID. You can look up any payer's ID in the Payer Network. Click on an error code to review a list of all the instances of that error.
This page helps you identify patterns in eligibility check failures. For example, if you see a large number of errors with code 75 (Subscriber/Insured Not Found) for a specific payer, you might want to investigate whether there are common issues with the patient data being submitted to that payer.
Visit Payer AAA errors for a complete list of AAA errors and their possible causes and resolutions.
Retry strategy
Implementing the right retry strategy for eligibility check failures saves a lot of time and money.
At a minimum, we strongly recommend automatically retrying every request that fails due to payer connectivity issues. Automatic retries resolve a significant portion of these types of failures without manual intervention.
Payer connectivity issues
We recommend implementing automatic retries for all of the following AAA error cases. These scenarios indicate temporary payer downtime, throttling, or intermittent connectivity issues:
42(Unable to Respond at Current Time)42(Unable to Respond at Current Time) and79(Invalid Participant Identification)80(No Response received - Transaction Terminated)
Our recommended retry strategy depends on your eligibility check workflow.
Real-time eligibility checks
For real-time eligibility checks that require a response within a few minutes, we recommend:
- Retry immediately and continue retrying for up to 2 minutes.
- The recommended retry window is based on what's acceptable in real-time human workflows. For example, a patient checking in for an appointment at their doctor's office.
- If the request is still unsuccessful, fail gracefully and escalate as needed.
Scheduled eligibility checks
You may want to run scheduled or background eligibility checks to perform periodic refreshes for a patient population or when checking eligibility for upcoming appointments.
If you're using the Batch Eligibility Check endpoint (recommended), Stedi automatically retries checks that fail due to payer connectivity issues for up to 8 hours.
If you're submitting real-time checks that can tolerate longer wait times, we recommend:
- Wait 1 minute to perform the first retry.
- Then, exponentially increase the wait between subsequent retries to up to 30 minutes between attempts.
- We recommend retrying for at least 8 hours, but the retry window should be based on your business workflows.
Other common error cases
You should also consider the following common error cases when implementing retries:
| AAA error | HTTP status | Reason | Retry Strategy |
|---|---|---|---|
| - | 429 | You exceeded your Stedi concurrency limit. | Retry immediately. Monitor your open concurrent requests and immediately replace any finished requests under your Stedi account limit. |
79 | 200 | Stedi successfully sent your request to the payer, but the payer rejected it. | First, retry as soon as possible with a different member and a different NPI. This helps determine whether the issue is with the original request or there is a broader issue with the payer. If you determine the issue is with the payer, follow our guidance for payer connectivity issues. |
79 | 400 | Either Stedi doesn't recognize the payer ID you provided, or the payer is not configured for eligibility checks. | Don't automatically retry. Fix the payer ID or contact Stedi support to resolve. |
Payer unable to find patient
Sometimes, a payer can't return benefits information for a patient even when the patient exists in their system. This problem can occur for a couple reasons.
Multiple matching records
Payers can have multiple records of patients with the same name and date of birth. The payer cannot return benefits information unless they are able to identify a unique match within their system.
To avoid this issue, we recommend:
- Include all of the demographic information available for a patient.
- Include the patient's member ID, if available.
Information discrepancies
There can be discrepancies between the information the provider has collected from the patient and the record the payer has in their system. These discrepancies can lead to issues returning a patient, even though a match exists. Some examples include differences in spelling the patient's name, using a nickname instead of the full name ("Nick" vs. "Nicolas"), and accidentally transposing numbers in the date of birth.
If a request fails to return the expected member in the response, we recommend progressively sending additional eligibility check requests with fewer patient identity and demographic data elements, or different combinations of those. This allows you to identify and handle cases where there are data errors or discrepancies between payer and provider data.
Name mismatches
If the payer fails to find a matching plan member due to a name mismatch, the errors array in the response typically has the code set to one of the following values:
65: Invalid/Missing Patient Name67: Patient Not Found73: Invalid/Missing Subscriber/Insured Name75: Subscriber/Insured Not Found
These error codes are set by the payer, not by Stedi, so it's possible that other error codes could be returned.
Resolving the error may require trying different name variations until the check is successful.
- Replace any nickname or shortened name with the full legal name, for example "Robert" instead of "Bob".
- Replace any non-English or accented characters (letters with diacritical marks) such as "Ñ" or "é" with the closest equivalent within the character restrictions. Stedi automatically replaces most such characters with the usual closest equivalent but this might not match the payer's record. For example, the character "Đ" could be transliterated to "D" or "J" depending on the romanization system used.
- For compound names try using only one or the other part. You can also try try removing the separator, or changing the separator from hyphen to space, or vice versa. Some payers may ignore special or separator characters when performing name searches.
- If the patient has recently changed their name, for example due to marriage, then the name stated by the patient or printed on their ID card might not match the payer's record. Try both the current and previous name.
Medi-Cal portal credentials
Medicaid California (Medi-Cal) is one of the few payers that require additional credentials to process eligibility checks.
When submitting eligibility checks to Medi-Cal, you must include the username and password the requesting provider uses to log into Medi-Cal's Provider Portal. These credentials will be different for each provider.
- JSON endpoint: Set the
portalUsernameandportalPasswordproperties. - Raw X12 endpoint: Include the portal credentials as
REFsegments withinLoop 2100B.- username:
REF02whenREF01is set toJD(User Identification) - password:
REF02whenREF01is set to4A(Personal Identification Number (PIN))
- username:
- Stedi portal: To add these fields to the New eligibility check form, click Select fields and check the boxes next to Portal username and Portal password.
If you don't include the provider's portal credentials or if the credentials are invalid, you'll receive an AAA error with code 41 (Authorization/Access Restrictions) at the payer or provider level.
Missing member ID
Our eligibility check endpoints require submitting at least one of the patient's member ID, date of birth, or last name in the request. However, some payers always require the member ID and reject requests without it.
Stedi tracks which payers require the member ID and returns a warning when you submit an eligibility check to one of those payers without it. The warning appears in the warnings array along with the AAA error from the payer in the errors array.
{
"warnings": [
{
"code": "request::270::member_id_required",
"description": "This payer requires the patient's member ID to be included in eligibility requests."
}
],
"errors": [
{
"code": "72",
"description": "Invalid/Missing Subscriber/Insured ID",
...
}
],
...
}Eligibility check requirements vary by payer. If we don't know whether a payer requires the member ID for eligibility checks, we don't return a warning.
Errors
You may encounter the following types of errors when submitting eligibility requests.
Stedi payer errors
Stedi returns errors when it encounters issues with the payer ID you provided.
| Error message | Possible causes and resolutions |
|---|---|
Payer is not configured for {transaction type}. Please contact Stedi support to resolve. | Stedi does not yet support this transaction type for this payer, or there is a mis-mapping of payer IDs. Contact us with the name of the payer, and we'll investigate the issue. |
Payer connection does not support {transaction type}. Please contact Stedi support to discuss connectivity options. | Stedi has a connection to this payer, but it doesn't currently support this functionality (real-time eligibility or claim submission). Contact us for a timeline on enabling it. |
Payer is not configured. Please check our published payer list or contact Stedi support to resolve. | Stedi doesn't recognize the payer ID you provided. Double-check the payer ID in the Stedi Payer Network, or contact us with the name of the payer, and we will help you determine the correct payer ID. |
Payer is not supported. Please contact Stedi support to discuss connectivity options. | Stedi doesn't yet have connectivity to this payer. We're likely already working on it - contact us for details about the connectivity timeline. |
The following error resulted from an unrecognized payer ID:
{
"meta": {
"outboundTraceId": "01KEJ02BRD3H716AP3HRBDM5Y8"
},
"controlNumber": "602859072",
"tradingPartnerServiceId": "AHS",
"errors": [
{
"code": "79",
"description": "Invalid Participant Identification",
"followupAction": "Please Correct and Resubmit",
"location": "2100A",
"possibleResolutions": "Payer AHS is not configured. Please check our published payer list or contact Stedi support to resolve."
}
],
"status": "ERROR",
"eligibilitySearchId": "019ba401-2f01-7262-a2b8-8707b70198c9",
"id": "ec_9d6a4f2b-1c7e-4e9a-b3f8-0a2c5e1d7b84"
}Validation errors
You may receive validation errors from Stedi or, rarely, from the payer.
Stedi
Stedi validates the structure of your eligibility request and won't submit your request to the payer if it's missing required fields or if the data is formatted incorrectly. The following Stedi validation error resulted from a missing required property:
{
"message": "Missing required field: provider npi, serviceProviderNumber, payorId, taxId, ssn, pharmacyProcessorNumber, servicesPlanID, or employersId is required",
"code": "BAD_REQUEST",
"eligibilitySearchId": "019ba403-e5ce-7181-8a2f-8cf093dde812",
"id": "ec_9d6a4f2b-1c7e-4e9a-b3f8-0a2c5e1d7b84"
}The following shows an example of a Stedi validation error resulting from an invalid date format:
{
"message": "subscriber.dateOfBirth: Provided date should be valid and in YYYYMMDD format.",
"code": "INVALID_REQUEST_BODY",
"eligibilitySearchId": "019ba405-e1ec-79e2-bde2-830664a901df",
"id": "ec_9d6a4f2b-1c7e-4e9a-b3f8-0a2c5e1d7b84"
}Payer (999 rejections)
Stedi's validation catches the majority of syntax and structural issues. However, some payers may occasionally return a 999 Implementation Acknowledgment indicating that the request was rejected.
Stedi can usually translate these 999 rejections into a more user-friendly 271 response with descriptive AAA errors in the errors array. When Stedi can't generate a 271, we return the raw 999 in the x12 property, set the status to ERROR, and include the number of EDI syntax errors in the implementationTransactionSetSyntaxError property. The errors array includes a general description indicating that the payer rejected the request due to validation errors.
The following example shows a 999 that resulted from sending the payer more than one STC code in the request:
{
"id": "ec_019c00bb-2293-7241-b283-9b94642b4ec4",
"transactionSetAcknowledgement": "R",
"tradingPartnerServiceId": "TESTPAYER",
"errors": [
{
"description": "The payer or intermediary clearinghouse rejected the request with validation errors. The original EDI response is returned in the `x12` field. Contact Stedi Support if you need further help."
}
],
"implementationTransactionSetSyntaxError": "5",
"controlNumber": "123456789",
"x12": "ISA*00* *00* *ZZ*STEDI *01*11234567890 *260127*1032*^*00501*000000000*0*P*:~GS*FA*STEDI*11234567890*20260127*1032*0*X*005010X231A1~ST*999*0001*005010X231A1~AK1*HS*1*005010X231A1~AK2*270*0001~IK3*EQ*12**8~IK4*1*0*5*32~IK5*R*5~AK9*R*1*1*0~SE*8*0001~GE*1*0~IEA*1*000000000~",
"meta": {
"outboundTraceId": "01KG0BP8NA69HK7095HE8XG03F"
},
"status": "ERROR",
"eligibilitySearchId": "019c00bb-229e-72c3-8585-8b28f0556a38"
}Payer AAA errors
When a payer rejects your eligibility check, the 271 response contains one or more AAA Request Validation segments that specify the reasons for the rejection and any recommended follow-up actions. Stedi includes this information in the aaaErrors object in the response JSON.
Common causes for AAA errors include:
- Missing or incorrect information for the subscriber, dependent, provider, or payer. In this case, you should correct any errors before resubmitting.
- Issues with payer enrollment. Many of these issues require that the provider contact the payer directly to resolve, due to PHI/HIPAA guidelines.
- The payer's system is down or experiencing issues. In this case, the payer may not have actually validated the data in your request. If you receive these types of errors, you should wait a few minutes and resend the request again.
Each error contains a followupAction:
- Please Correct and Resubmit
- Resubmission Not Allowed | Note that this code doesn't mean you should never resubmit the request. Intermediary clearinghouses may send this code when they have temporarily lost connection to the payer, so this code indicates that you should wait at least a few minutes before retrying instead of retrying immediately.
- Resubmission Allowed
- Do Not Resubmit; Inquiry Initiated to a Third Party | This code is uncommon
- Please Resubmit Original Transaction
- Please Wait 30 Days and Resubmit | This code is uncommon
- Please Wait 10 Days and Resubmit | This code is uncommon
- Do not resubmit; We Will Hold Your Request and Respond Again Shortly | This code is uncommon
AAA errors can be present at multiple different levels in the response, depending on the type. The following example shows an error at the subscriber level (subscriber.aaaErrors):
{
"subscriber": {
"memberId": "123456789",
"firstName": "JANE",
"lastName": "DOE",
"entityIdentifier": "Insured or Subscriber",
"entityType": "Person",
"dateOfBirth": "19001103",
"aaaErrors": [
{
"field": "AAA",
"code": "75",
"description": "Subscriber/Insured Not Found",
"followupAction": "Please Correct and Resubmit",
"location": "Loop 2100C",
"possibleResolutions": "- Subscriber was not found."
}
]
}
}However, all errors at the payer, provider, subscriber, and dependents levels are also reported in the top-level errors array in the eligibility check response.
Visit Eligibility mock requests to retrieve more examples of common AAA errors in eligibility responses.
To help with troubleshooting, we include additional strings containing
possible causes and resolutions for each AAA error. We periodically update
this guidance, so these strings may change at any time and may differ between
eligibility responses. Don't build programmatic logic that depends on
matching these strings exactly.
Payer
You may receive the following types of errors at the payer level.
| Code | Description | Possible causes and resolutions |
|---|---|---|
04 | Authorized Quantity Exceeded | You included too many patients in the request - you can only request benefits information for one patient at a time.
|
41 | Authorization/Access Restrictions | The problem is either:
|
42 | Unable to Respond at Current Time | The payer can't respond to your request. This is typically a temporary issue with the payer's system, such as downtime, but it can also be an extended outage. We recommend retrying immediately and continuing to retry for up to 2 minutes. Learn more about our recommended retry strategy for payer connectivity issues. |
79 | Invalid Participant Identification | There is a problem connecting with this payer. Contact Stedi support. |
80 | No Response received - Transaction Terminated | The payer can't respond to your request. This is typically a temporary issue with the payer's system, such as downtime, but it can also be an extended outage. We recommend retrying immediately and continuing to retry for up to 2 minutes. Learn more about our recommended retry strategy for payer connectivity issues. |
T4 | Payer Name or Identifier Missing | The problem is either:
|
Provider
You may receive the following types of errors at the provider level.
| Code | Description | Possible causes and resolutions |
|---|---|---|
15 | Required application data missing | The payer needs more information about the provider requesting the eligibility check. Try including the provider.taxId, typically their EIN or SSN. |
41 | Authorization/Access Restrictions | The problem is either:
|
43 | Invalid/Missing Provider Identification | The problem is either:
|
44 | Invalid/Missing Provider Name | The provider's NPI is registered with an incorrect name for this payer.
|
45 | Invalid/Missing Provider Specialty | The provider's NPI isn't registered with the payer under the correct specialty. The provider must contact the payer directly to resolve this issue due to PHI/HIPAA guidelines. The payer may require other credentialing or enrollment processes. |
46 | Invalid/Missing Provider Phone Number | The provider's phone number doesn't match the one registered with the payer or the one in the NPPES system. The provider must contact the payer directly to resolve this issue because of PHI/HIPAA guidelines. The payer may require other credentialing or enrollment processes. |
47 | Invalid/Missing Provider State | The provider.address either doesn't match the address registered with the payer or it doesn't match the provider's address in the NPPES system.
|
48 | Invalid/Missing Referring Provider Identification Number | The referring provider (specified in subscriber.providerIdentifier) either:
|
50 | Provider Ineligible for Inquiries | The provider requesting the eligibility check isn't registered with the payer for the service type in encounter.serviceTypeCodes.
|
51 | Provider Not on File | The provider isn't registered with the payer.
|
79 | Invalid Participant Identification | There is a problem connecting with this payer. Contact Stedi support. |
97 | Invalid or Missing Provider Address | The payer requires the address for the provider requesting the eligibility check. Retry with the provider's complete address in the provider.address object. |
T4 | Payer Name or Identifier Missing | The problem is either:
|
Subscriber
You may receive the following types of errors at the subscriber level.
| Code | Description | Possible causes and resolutions |
|---|---|---|
15 | Required application data missing |
|
33 | Input Errors | The request doesn't meet the payer’s requirements, which usually means it doesn't contain enough information to identify the patient. We recommend providing the subscriber's memberId, dateOfBirth, firstName, and lastName. Given this information, all payers must return benefits details as long as they can find a unique match for the member within their system. Visit patient information to learn more. |
35 | Out of Network | The subscriber isn't in the provider's network.
|
42 | Unable to Respond at Current Time | The payer can't respond to your request. This is typically a temporary issue with the payer's system, such as downtime, but it can also be an extended outage. We recommend retrying immediately and continuing to retry for up to 2 minutes. Learn more about our recommended retry strategy for payer connectivity issues. |
43 | Invalid/Missing Provider Identification | The problem is either:
|
45 | Invalid/Missing Provider Specialty | The provider.npi isn't registered with the payer under the correct specialty. The provider must contact the payer directly to resolve this issue due to PHI/HIPAA guidelines. |
47 | Invalid/Missing Provider State | The provider.address either doesn't match the address registered with the payer, or it doesn't match the provider's address in the NPPES system.
|
48 | Invalid/Missing Referring Provider Identification Number | The referring provider (specified in subscriber.providerIdentifier) either:
|
49 | Provider is Not Primary Care Physician | The payer doesn’t list the provider as a primary care physician but requires them to be one. The provider or the patient must contact the payer to update their records. |
51 | Provider Not on File | The provider isn't registered with the payer.
|
52 | Service Dates Not Within Provider Plan Enrollment | The provider wasn't registered with the patient's health plan on the date of service listed in the eligibility check.
|
53 | Inquired Benefit Inconsistent with Provider Type Enrollment | The provider isn't registered with the payer to perform the requested benefit type. Some payers only return benefits that match the provider's taxonomy code.
|
54 | Inappropriate Product/Service ID Qualifier | You provided an invalid encounter.productOrServiceIDQualifier. Update the request and resubmit. |
55 | Inappropriate Product/Service ID | You provided an invalid encounter.procedureCode. Update the request and resubmit. |
56 | Inappropriate Date | The service dates in the encounter object are incorrect or are formatted incorrectly. .
|
57 | Invalid/Missing Date(s) of Service | The service dates in the encounter object are missing, incorrect, or formatted incorrectly.
|
58 | Invalid/Missing Date-of-Birth | The payer needs the subscriber's date of birth for identification.
|
60 | Date of Birth Follows Date(s) of Service | The date(s) of service you provided are earlier than the subscriber's date of birth.
|
61 | Date of Death Precedes Date(s) of Service | The date(s) of service you provided are after the patient's date of death.
|
62 | Date of Service Not Within Allowable Inquiry Period | The payer doesn't support the date(s) of service you provided.
|
63 | Date of Service in Future | Some payers don't support future date(s) of service.
|
69 | Inconsistent with Patient’s Age | The diagnosis codes provided don't match the patient's age.
|
70 | Inconsistent with Patient’s Gender | The procedure codes provided are inconsistent with the patient's gender.
|
71 | Patient Birth Date Does Not Match That for the Patient on the Database | The subscriber's birth date doesn't match what's in the payer's database.
|
72 | Invalid/Missing Subscriber/Insured ID | The subscriber's member ID is either missing or invalid.
|
73 | Invalid/Missing Subscriber/Insured Name | The payer doesn't recognize the subscriber's name.
|
74 | Invalid/Missing Subscriber/Insured Gender Code | The payer requires the subscriber's gender code. Ensure subscriber.gender is set to a valid value that matches the payer's records. |
75 | Subscriber/Insured Not Found | The payer couldn't locate the subscriber in their database.
|
76 | Duplicate Subscriber/Insured ID Number | The payer found another member with the same member ID in their database. Ensure the subscriber.memberId is correct. |
78 | Subscriber/Insured Not in Group/Plan identified | The subscriber isn't in the specified health plan.
|
98 | Experimental Service or Procedure | Contact the payer for guidance. |
Aa | Authorization Number Not Found | The prior authorization number the payer has on file doesn't match the one you sent. Verify that the encounter.priorAuthorizationOrReferralNumber is correct. |
AE | Requires Primary Care Physician Authorization | The payer requires a prior authorization number. Add the encounter.priorAuthorizationOrReferralNumber to your request and resubmit. |
AF | Invalid/Missing Diagnosis Code(s) | The payer requires one or more diagnosis codes, or the diagnosis codes you provided are invalid. Ensure the information in the subscriber.healthCareCodeInformation[] array is correct. |
AG | Invalid/Missing Procedure Code(s) | The payer requires a procedure code or the procedure code you provided is invalid. Ensure encounter.productOrServiceIDQualifier and encounter.procedureCode are set to valid values. |
AO | Additional Patient Condition Information Required | Contact the payer for guidance. |
CI | Certification Information Does Not Match Patient | The prior authorization number the payer has on file doesn't match the one you sent. Verify that the encounter.priorAuthorizationOrReferralNumber is correct. |
E8 | Requires Medical Review | Contact the payer for guidance. |
IA | Invalid Authorization Number Format | The encounter.priorAuthorizationOrReferralNumber wasn't formatted correctly. |
MA | Missing Authorization Number | You must include a previously issued referral or authorization number in your request. Set the encounter.referenceIdentificationQualifier and encounter.priorAuthorizationOrReferralNumber properties and resubmit. |
Dependents
You may receive the following errors at the dependents level.
| Code | Description | Possible causes and resolutions |
|---|---|---|
15 | Required application data missing |
|
33 | Input Errors | The request doesn't meet the payer’s requirements, which usually means it doesn't contain enough information to identify the patient.
|
35 | Out of Network | The dependent isn't in the provider's network.
|
42 | Unable to Respond at Current Time | The payer can't respond to your request. This is typically a temporary issue with the payer's system, such as downtime, but it can also be an extended outage. We recommend retrying immediately and continuing to retry for up to 2 minutes. Learn more about our recommended retry strategy for payer connectivity issues. |
43 | Invalid/Missing Provider Identification | The problem is either:
|
45 | Invalid/Missing Provider Specialty | The provider.npi isn't registered with the payer under the correct specialty. The provider must contact the payer directly to resolve this issue due to PHI/HIPAA guidelines. |
47 | Invalid/Missing Provider State Specialty | The provider.address either doesn't match the address registered with the payer, or it doesn't match the provider's address in the NPPES system.
|
48 | Invalid/Missing Referring Provider Identification Number | The referring provider (specified in dependents[].providerIdentifier) either:
|
49 | Provider is Not Primary Care Physician | The payer doesn't list the provider as a primary care physician, but requires them to be one. The provider or the patient must contact the payer to update their records. |
51 | Provider Not on File | The provider isn't registered with the payer.
|
52 | Service Dates Not Within Provider Plan Enrollment | The provider wasn't registered with the patient's health plan on the date of service listed in the eligibility check.
|
53 | Inquired Benefit Inconsistent with Provider Type Enrollment | The provider isn't registered with the payer to perform the requested benefit type. Some payers only return benefits that match the provider's taxonomy code.
|
54 | Inappropriate Product/Service ID Qualifier | You provided an invalid encounter.productOrServiceIDQualifier. Update the request and resubmit. |
55 | Inappropriate Product/Service ID | You provided an invalid encounter.procedureCode. Update the request and resubmit. |
56 | Inappropriate Date | The service dates in the encounter object are incorrect or are formatted incorrectly.
|
57 | Invalid/Missing Date(s) of Service | The service dates in the encounter object are missing, incorrect, or formatted incorrectly.
|
58 | Invalid/Missing Date-of-Birth | The payer needs the dependent's date of birth for identification.
|
60 | Date of Birth Follows Date(s) of Service | The date(s) of service you provided are earlier than the dependent's date of birth.
|
61 | Date of Death Precedes Date(s) of Service | The date(s) of service you provided are after the dependent's date of death.
|
62 | Date of Service Not Within Allowable Inquiry Period | The payer doesn't support the date(s) of service you provided.
|
63 | Date of Service in Future | Some payers don't support future date(s) of service.
|
64 | Invalid/Missing Patient ID | The payer requires an additional identifier in the dependents[].additionalIdentification object.
|
65 | Invalid/Missing Patient Name | The payer doesn't recognize the dependent's name.
|
66 | Invalid/Missing Patient Gender Code | The payer requires the dependent's gender code. Ensure dependents[].gender is set to a valid value that matches the payer's records. |
67 | Patient Not Found | The payer couldn't locate the dependent in their database.
|
68 | Duplicate Patient ID Number | The payer found another member with the same member ID in their database. Ensure the subscriber.memberId is correct. |
69 | Inconsistent with Patient’s Age | The diagnosis codes provided don't match the patient's age.
|
70 | Inconsistent with Patient’s Gender | The procedure codes provided are inconsistent with the patient's gender.
|
71 | Patient DOB Does Not Match That for the Patient on the Database | The dependent's birth date doesn't match what's in the payer's database.
|
77 | Subscriber Found, Patient Not Found | The payer identified the subscriber in their database, but not the dependent.
|
98 | Experimental Service or Procedure | Contact the payer for guidance. |
AA | Authorization Number Not Found | The payer didn't recognize the prior authorization number you provided. Ensure the encounter.priorAuthorizationOrReferralNumber is correct. |
AE | Requires Primary Care Physician Authorization | The payer requires a prior authorization number. Add the encounter.priorAuthorizationOrReferralNumber to your request and resubmit. |
AF | Invalid/Missing Diagnosis Code(s) | The payer requires diagnosis codes, or the diagnosis codes you provided were invalid. Ensure the information in the dependents[].healthCareCodeInformation[] array is correct. |
AG | Invalid/Missing Procedure Code(s) | The payer requires a procedure code or the procedure code you provided is invalid. Ensure encounter.productOrServiceIDQualifier and encounter.procedureCode are set to valid values. |
AO | Additional Patient Condition Information Required | Contact the payer for guidance. |
CI | Certification Information Does Not Match Patient | The prior authorization or referral number the payer has on file for the patient doesn't match the one you sent. Verify that the encounter.priorAuthorizationOrReferralNumber is correct. |
E8 | Requires Medical Review | Contact the payer for guidance. |
IA | Invalid Authorization Number Format | The encounter.priorAuthorizationOrReferralNumber wasn't formatted correctly. |
MA | Missing Authorization Number | You must include a previously issued referral or authorization number in your request. Set the encounter.referenceIdentificationQualifier and encounter.priorAuthorizationOrReferralNumber properties and resubmit. |
Card Issuer Identifier (80840)
All health plans use (80840) as the first five digits of the Card Issuer Identifier.
This is a placeholder value used for standards compliance only, and you shouldn't pass it in an electronic eligibility check. However, many providers and OCR systems accidentally pass (80840) in other eligibility check fields. For example, they may try to pass this value as a subscriber or dependent ID, causing an AAA rejection from the payer.
To prevent these types of mistakes, Stedi automatically suppresses any string containing (80840) in the following fields:
| JSON | X12 EDI |
|---|---|
subscriber.memberId | Loop 2100C NM109 Subscriber Primary Identifier |
Any property in subscriber.additionalIdentification | Loop 2100C REF02 Subscriber Supplemental Identifier |
Any property in dependent.additionalIdentification | Loop 2100D REF02 Dependent Supplemental Identifier |
If the payer's eligibility response returns an AAA error, Stedi returns the following warning:
The field {FIELD} contains the string "(80840)", which is a known
placeholder prefix for a field that should not be provided in {FIELD}.
We have omitted that value in the request, and the request failed.
Please locate the correct value for {FIELD} and resubmit.To correct this error, read the documentation for the corresponding field, locate the correct value, and resubmit the eligibility check.
SOAP requests
Our Real-Time Eligibility Check SOAP endpoint respects the error handling rules defined in the CAQH CORE vC2.2.0 Rule.
At a high level, you can experience errors in the following categories:
- Authentication errors: Either your API key, your Stedi account ID, or both are invalid.
- SOAP faults: Issues with the request
EnvelopeorHeaderelements, such as malformed XML. - CORE-compliant errors: The request don't conform to CAQH CORE rules for eligibility checks.
- X12 EDI validation errors: The X12 EDI transaction doesn't match the required format.
- Too many requests errors: You've exceeded your concurrency limit.
- Payer
AAAerrors: Errors from the payer indicating issues with processing your request.
Authentication errors
If the wsse:Username or wsse:Password values are incorrect within the Header element:
- Stedi returns an HTTP
401status code. - The response includes an
ErrorCodeelement set toUnAuthorized.
The following example shows an authentication error response:
<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope">
<soapenv:Body>
<COREEnvelopeRealTimeResponse>
<PayloadType>CoreEnvelopeError</PayloadType>
<ProcessingMode>RealTime</ProcessingMode>
<PayloadID>01987b7e-56cc-7871-8520-a22721948fb4</PayloadID>
<TimeStamp>2025-08-06T22:23:50Z</TimeStamp>
<CORERuleVersion>2.2.0</CORERuleVersion>
<Payload></Payload>
<ErrorCode>UnAuthorized</ErrorCode>
<ErrorMessage>Invalid username and/or password.</ErrorMessage>
</COREEnvelopeRealTimeResponse>
</soapenv:Body>
</Envelope>SOAP faults
SOAP faults indicate issues with the request Envelope or Header elements, such as malformed XML or missing required elements.
When these errors occur:
- Stedi returns an HTTP
400status code. - The response includes a
Faultelement that contains details about the error. TheFaultelement always contains aCodeandReasonelement. TheCodeelement indicates the source of the error and theReasonelement provides a description.
The following example shows a SOAP fault response:
<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope/" xmlns:xsd="http://www.w3.org/2001/XMLSchema"
xmlns:xsi="http://www.w3.org/2001/XMLSchema-instance">
<soapenv:Body>
<soapenv:Fault>
<soapenv:Code>
<soapenv:Value>soapenv:Sender</soapenv:Value>
</soapenv:Code>
<soapenv:Reason>
<soapenv:Text xml:lang="en">Unable to parse payload as CORE SOAP request</soapenv:Text>
</soapenv:Reason>
</soapenv:Fault>
</soapenv:Body>
</soapenv:Envelope>Visit the SOAP Fault documentation for more details and a complete list of possible error codes.
CORE-compliant errors
These errors typically indicate issues with the COREEnvelopeRealTimeRequest element that contains the request body. However, they can sometimes indicate specific issues with the SOAP Envelope or Header elements, such as an incorrect SOAP version or invalid credentials.
When these errors occur:
- Stedi returns an HTTP
400status code. - The
COREEnvelopeRealTimeResponseelement contains anErrorCodeandErrorMessagewith a description. - The
Payloadelement is empty because Stedi didn't process the eligibility check.
The following example shows a CORE-compliant error response:
<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope">
<soapenv:Body>
<COREEnvelopeRealTimeResponse>
<PayloadType>CoreEnvelopeError</PayloadType>
<ProcessingMode>RealTime</ProcessingMode>
<PayloadID>01987b70-2b7e-7b40-9875-10d3139dcf2a</PayloadID>
<TimeStamp>2025-08-06T22:23:50Z</TimeStamp>
<SenderID>TestStedi</SenderID>
<ReceiverID>Stedi</ReceiverID>
<CORERuleVersion>2.2.0</CORERuleVersion>
<Payload></Payload>
<ErrorCode>PayloadIDIllegal</ErrorCode>
<ErrorMessage>Illegal value provided for PayloadID. Must be a valid UUID</ErrorMessage>
</COREEnvelopeRealTimeResponse>
</soapenv:Body>
</soapenv:Envelope>The following table lists the possible values for ErrorCode and and their causes:
| Error Code | Possible Causes |
|---|---|
CORERuleVersionIllegal | The CORERuleVersion element is not set to 2.2.0. |
CORERuleVersionRequired | The CORERuleVersion element is missing from the request. Set this to 2.2.0. |
PayloadIDIllegal | The PayloadID element is not a valid UUID. |
PayloadIDRequired | The PayloadID element is missing from the request. This must be a valid UUID. |
PayloadIllegal | The Payload element is empty or doesn't contain a valid X12 EDI 270 transaction. |
PayloadRequired | The Payload element is missing from the request. This must be a valid X12 EDI 270 transaction. |
PayloadTypeIllegal | The PayloadType element is invalid. Set this to X12_270_Request_005010X279A1. |
PayloadTypeRequired | The PayloadType element is missing from the request. Set this to X12_270_Request_005010X279A1. |
ProcessingModeIllegal | The ProcessingMode element is not set to RealTime. |
ProcessingModeRequired | The ProcessingMode element is missing from the request. Set this to RealTime for real-time eligibility checks. |
ReceiverIDIllegal | The ReceiverID exceeds the maximum length of 50 characters. |
ReceiverIDRequired | The ReceiverID element is missing from the request. Visit the Request reference documentation for guidance on which identifier to use. |
SenderIDIllegal | The SenderID exceeds the maximum length of 50 characters. |
SenderIDRequired | The SenderID element is missing from the request. Visit the Request reference documentation for guidance on which identifier to use. |
TimeStampIllegal | The TimeStamp element is not in the correct format. It must be in ISO 8601 format, such as 2024-07-28T12:00:00Z. |
TimeStampRequired | The TimeStamp element is missing from the request. |
UnAuthorized | The request is unauthorized. This can happen if the wsse:UsernameToken is missing or invalid, or if the API key is incorrect. |
VersionMismatch | The SOAP version in the request does not match the expected version. |
X12 EDI validation errors
Validation errors occur when the X12 EDI transaction doesn't conform to the expected 270 X12 EDI format or contains invalid data.
When there are validation errors, Stedi returns an HTTP 400 status code. There are two possible error cases:
- Invalid EDI envelope: There are issues with the
ISAorGSheader. TheErrorCodeelement is set toPayloadIllegal, and thePayloadelement is empty because Stedi couldn't parse the request.<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope"><soapenv:Body> <COREEnvelopeRealTimeResponse> <PayloadType>CoreEnvelopeError</PayloadType> <ProcessingMode>RealTime</ProcessingMode> <PayloadID>01987c0b-c8b3-71c1-bd6f-8e26725c7110</PayloadID> <TimeStamp>2025-08-06T22:23:50Z</TimeStamp> <SenderID>RECEIVER-ID</SenderID> <ReceiverID>SENDER-ID</ReceiverID> <CORERuleVersion>2.2.0</CORERuleVersion> <Payload></Payload> <ErrorCode>PayloadIllegal</ErrorCode> <ErrorMessage>Error while getting metadata for an X12 file: Error reading EDI: Invalid ISA: ISA-11 must be 'U' for interchange control versions earlier than 00402</ErrorMessage> </COREEnvelopeRealTimeResponse> </soapenv:Body> </soapenv:Envelope> - Invalid EDI transaction: Stedi successfully parsed the EDI envelope, but there are validation issues with the rest of the transaction. The
ErrorCodeelement is set toSuccess, and thePayloadelement contains a 999 Implementation Acknowledgment describing the errors. This 999 is usually from Stedi, but it can also be from the payer.<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope"> <soapenv:Body> <COREEnvelopeRealTimeResponse> <PayloadType>X12_999_Response_005010X231A1</PayloadType> <ProcessingMode>RealTime</ProcessingMode> <PayloadID>01987c11-ae2e-7f63-801d-cb3529f45952</PayloadID> <TimeStamp>2025-08-06T22:23:50Z</TimeStamp> <SenderID>RECEIVER-ID</SenderID> <ReceiverID>SENDER-ID</ReceiverID> <CORERuleVersion>2.2.0</CORERuleVersion> <Payload><![CDATA[ISA*00* *00* *ZZ*RECEIVER *ZZ*SENDER *250806*1910*^*00501*000000001*0*T*:~GS*FA*STEDI*117151744*20250806*191051*10*X*005010X231A1~ST*999*0001*005010X231A1~AK1*HS*1*005010X279A1~AK2*270*1234*005010X279A1~IK3*BHT*2**8~IK4*4*373*8*20240321!1319~IK4*5**1~IK3*BHT*2**8~IK4*4*373*8*20240321!1319~IK4*5**1~IK5*R*5~AK9*R*1*1*0~SE*12*0001~GE*1*10~IEA*1*000000001~]]></Payload> <ErrorCode>Success</ErrorCode> <ErrorMessage/> </COREEnvelopeRealTimeResponse> </soapenv:Body> </soapenv:Envelope>
Too many requests
If you exceed your concurrency limit for the SOAP endpoint:
- Stedi returns an HTTP
429status code. - The X12 EDI transaction inside the
Payloadelement contains anAAAerror with code42.
Stedi will continue rejecting additional requests with a 429 status code until one of your previous requests is completed.
The following example shows a too many requests response:
<soapenv:Envelope xmlns:soapenv="http://www.w3.org/2003/05/soap-envelope">
<soapenv:Body>
<COREEnvelopeRealTimeResponse>
<PayloadType>X12_271_Response_005010X279A1</PayloadType>
<ProcessingMode>RealTime</ProcessingMode>
<PayloadID>019afed8-aa83-7fe2-a1bf-18dd5942a772</PayloadID>
<TimeStamp>2025-12-08T16:43:23Z</TimeStamp>
<SenderID>STEDI</SenderID>
<ReceiverID>686460348755</ReceiverID>
<CORERuleVersion>2.2.0</CORERuleVersion>
<Payload><![CDATA[ISA*00* *00* *ZZ*STEDI ...*AAA*Y**42*R*...]]></Payload>
<ErrorCode>Success</ErrorCode>
<ErrorMessage> </ErrorMessage>
</COREEnvelopeRealTimeResponse>
</soapenv:Body>
</soapenv:Envelope>