Automate claim submission
Reduce administrative work and avoid unnecessary delays. Our APIs have built-in validation and repair—commonly referred to as “edits”—for fewer payer rejections.
Track outstanding claims
Keep patients and providers informed with real-time claim status updates.
Streamline issue resolution
Quickly identify and address underpayments, denials, and disputes.
Ingest ERAs
Automatically ingest electronic remittances to keep your financial ledger up to date and get paid faster.
How it works
Integrate with a modern, developer-friendly API
Claim submission
Submit Professional (837P), Dental (837D), and Institutional (837I) claims to thousands of payers. Stedi creates a HIPAA-compliant transaction, applies enhanced edits, and sends it to the right payer.
submitClaim.js
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
getClaimStatus.js
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
Real-time claim status
Check any claim’s status in seconds with our Claim Status API. Receive status responses in easily digestible JSON.
Electronic remittance advice (ERAs)
Receive ERAs automatically through Stedi webhooks or periodically poll for new transactions.
electronicRemittanceAdvice.json
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
getClaimStatus.js
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
Claim attachments
Programmatically upload PDFs and images to Stedi. Then send 275 claim attachments for 837P, 837D, and 837I claims.
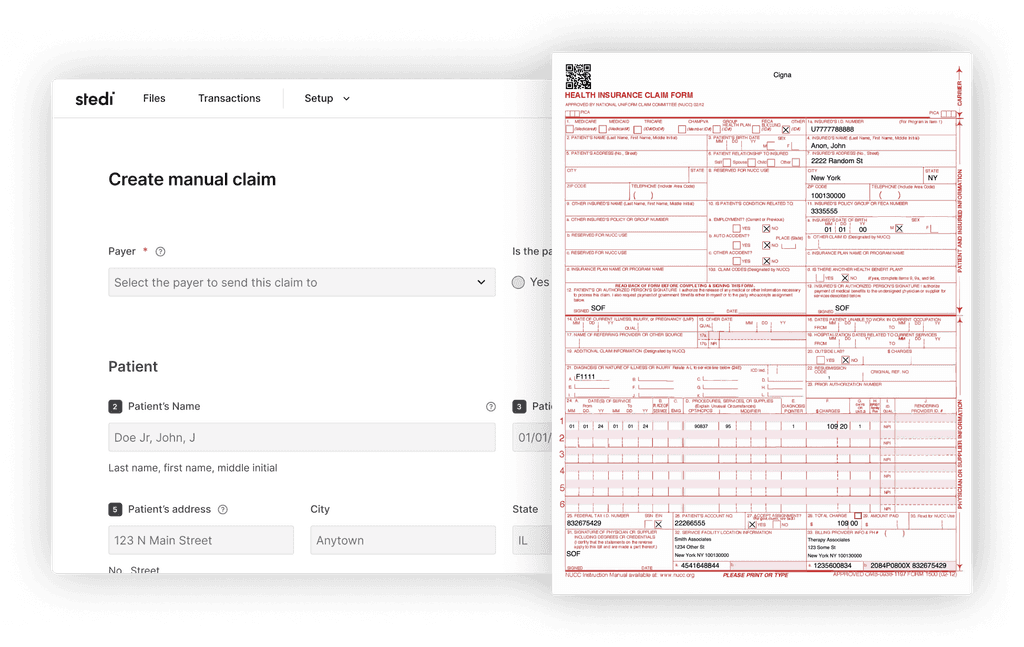
Manual claim submission
Test integrations and review claims in a familiar format
Submit claims through a digital version of the CMS-1500 Claim Form. Get auto-generated CMS-1500 PDFs through the app or API.
Connect to thousands of payers
Our growing set of payers provide broad, reliable connectivity.
Automatic failover
Stedi dynamically routes traffic to the most reliable connection, eliminating single points of failure, providing redundant connections.