Introducing Stedi Transaction Enrollment: An API-first approach to managing enrollments
Dec 17, 2024
Products
All payers require providers to complete an enrollment process before they can start receiving claim remittances (ERAs). Though less common, certain payers also require enrollment before allowing providers to submit transactions like claims and eligibility checks.
The typical enrollment process is highly manual and notoriously painful. There are no APIs or uniform standards, so every payer has different requirements. Forms, online portals, PDFs, wet signatures, and even fax machines can all be part of the process, causing significant frustration and slowing down the overall revenue cycle. After the enrollment is submitted, it’s a black box; days or weeks go by with no status updates, forcing providers to wait to submit claims, check patient eligibility, and receive information about payments. These issues compound for revenue cycle management companies that do hundreds or thousands of enrollments on behalf of many providers.
That’s why Stedi designed a new enrollment experience from the ground up. Through Stedi's user-friendly interface or modern API, developers and operations teams can now submit enrollments for specific transaction types in a streamlined flow – either one at a time or in large batches.
Once you submit an enrollment request, Stedi manages the entire process for you, including submitting the enrollment to the payer, following up as needed, and giving clear guidance for any additional steps that might be required. You can monitor the enrollment status throughout the process using the API or our searchable Enrollments dashboard.
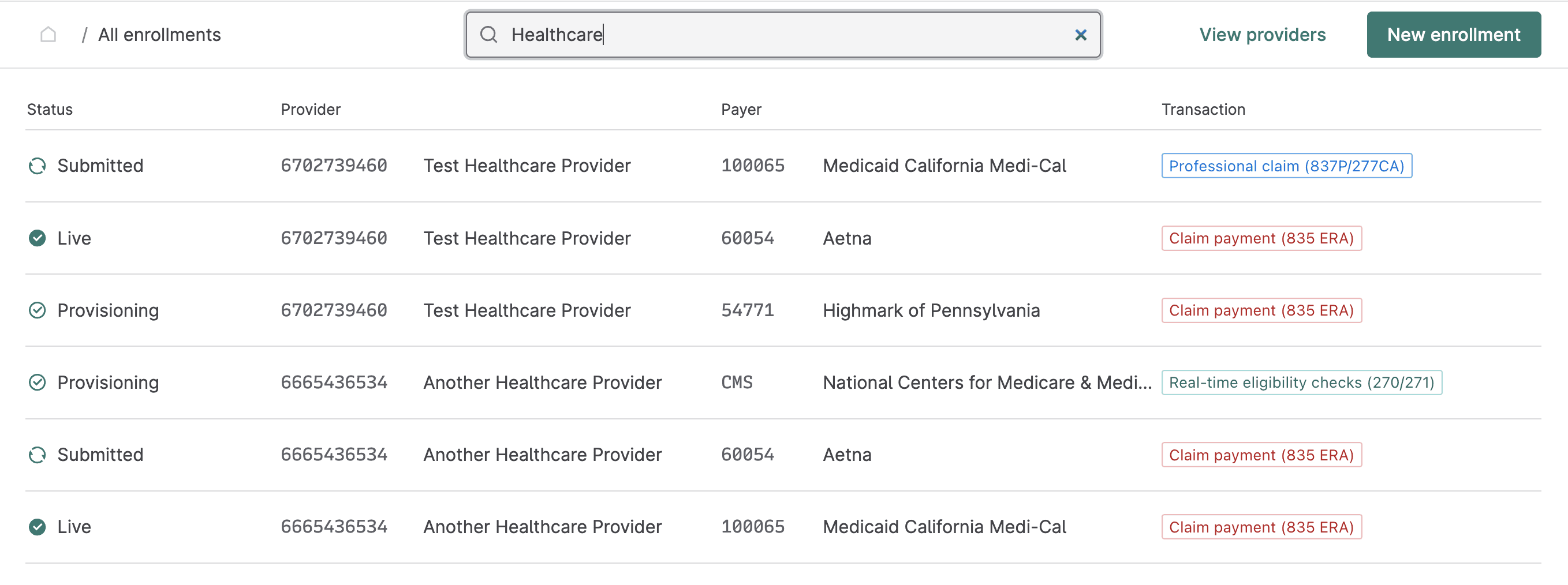
Manage transaction enrollments through Stedi’s user-friendly app or APIs
You can submit and monitor all of your organization’s transaction enrollments from the Enrollments page in Stedi. For each enrollment request, Stedi displays the provider, status, payer, and transaction type. You can click any enrollment request to view its complete details, including any notes from Stedi regarding the next steps.
You can also manage the entire transaction enrollment process programmatically through Stedi’s Transaction Enrollment API. This approach is especially useful when you need to perform bulk enrollments for many providers at once, or when you want to embed enrollment capabilities into your own application. The following example request enrolls a provider for claim payments (835 ERAs) with UnitedHealthcare (Payer ID: 87726).
curl --request POST \
--url https://enrollments.us.stedi.com/2024-09-01/enrollments \
--header 'Authorization: <api-key>' \
--header 'Content-Type: application/json' \
--data '{
"transactions": {
"claimPayment": {
"enroll": true
}
},
"primaryContact": {
"firstName": "John",
"lastName": "Doe",
"email": "test@example.com",
"phone": "555-123-34354",
"streetAddress1": "123 Some Str.",
"city": "A City",
"state": "MD",
"zipCode": "20814"
},
"userEmail": "test@example.com",
"payer": {
"id": "87726"
},
"provider": {
"id": "db6665c5-7b97-4af9-8c68-a00a336c2998"
}
}'Streamlined processing
Transaction enrollment requests you submit manually and programmatically follow the same streamlined process:
Add provider: You add a new provider record with the information required for enrollment, including the provider's name, tax ID, NPI, and contact information.
Submit transaction enrollment requests: You submit requests to enroll the provider with required payers, one for each transaction type. For example, you’d submit three separate requests to enroll a provider for 837P (professional) claims, 270 real-time eligibility checks, and 835 ERAs (claim payments). You can save requests in
DRAFTstatus until you're ready to submit them to Stedi. Once you submit an enrollment request, its status is set toSUBMITTED, and it enters Stedi’s queue for processing.Provisioning: Stedi begins the enrollment process with the payer and sets the enrollment request status to
PROVISIONING. Our team leaves clear instructions about what to do next, if required, and provides hands-on help as needed with additional steps.Enrollment is Live: Once the enrollment is approved, the enrollment request status is set to
LIVE, and the provider can start exchanging the enrolled transactions with the payer.
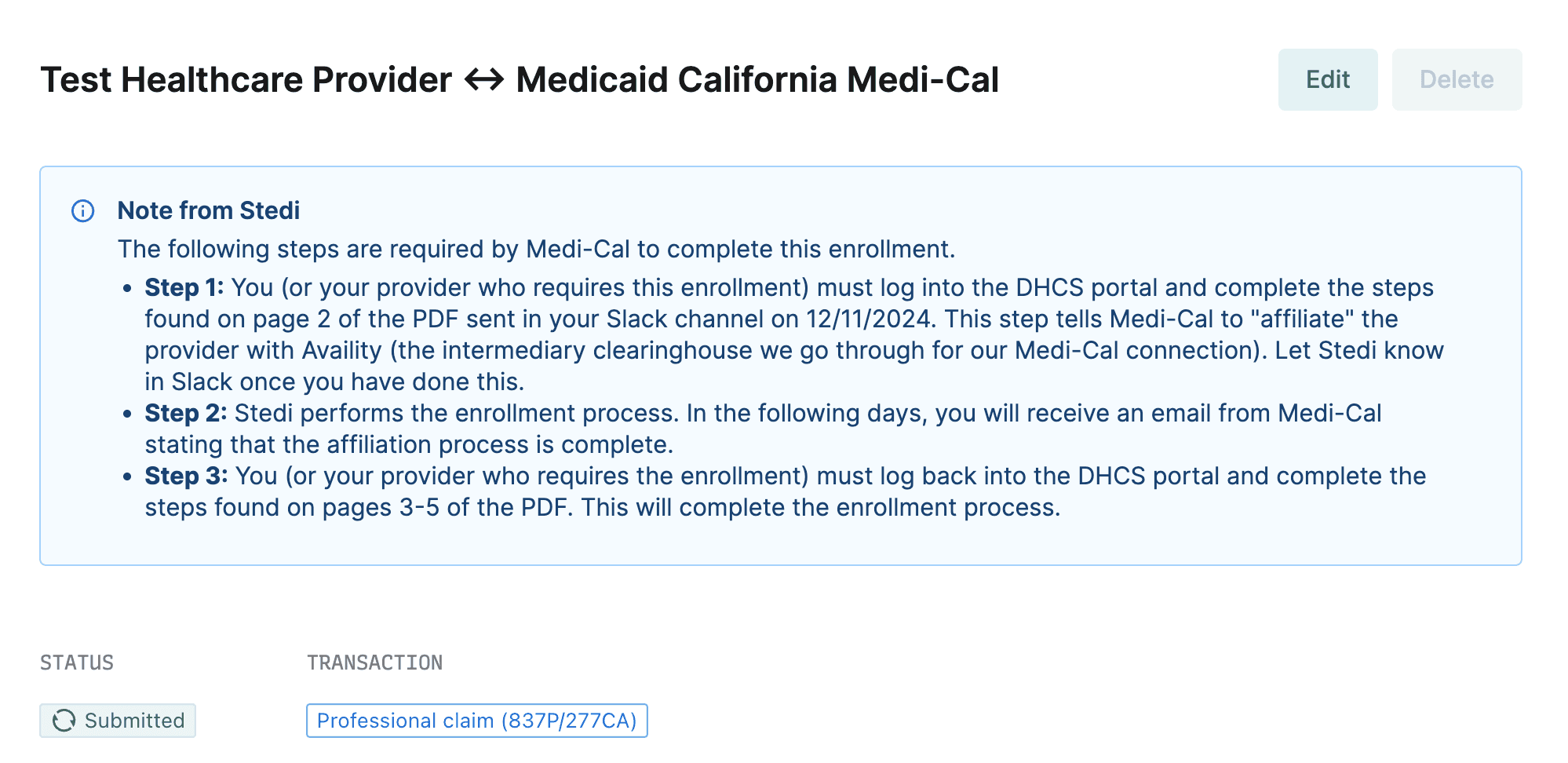
Clear status updates and expert guidance
Our customer success team knows the nuances of each payer’s enrollment requirements and breaks them down into clear, actionable steps. In addition to updating your enrollment request with any action items required for your team, we also reach out to you in your dedicated Slack channel with resources and to answer any follow-up questions.
The following example shows an enrollment request for Medicaid California Medi-Cal that requires additional steps for the provider. In Step 1, customer support notes that they dropped the required PDF in Slack for easy access.
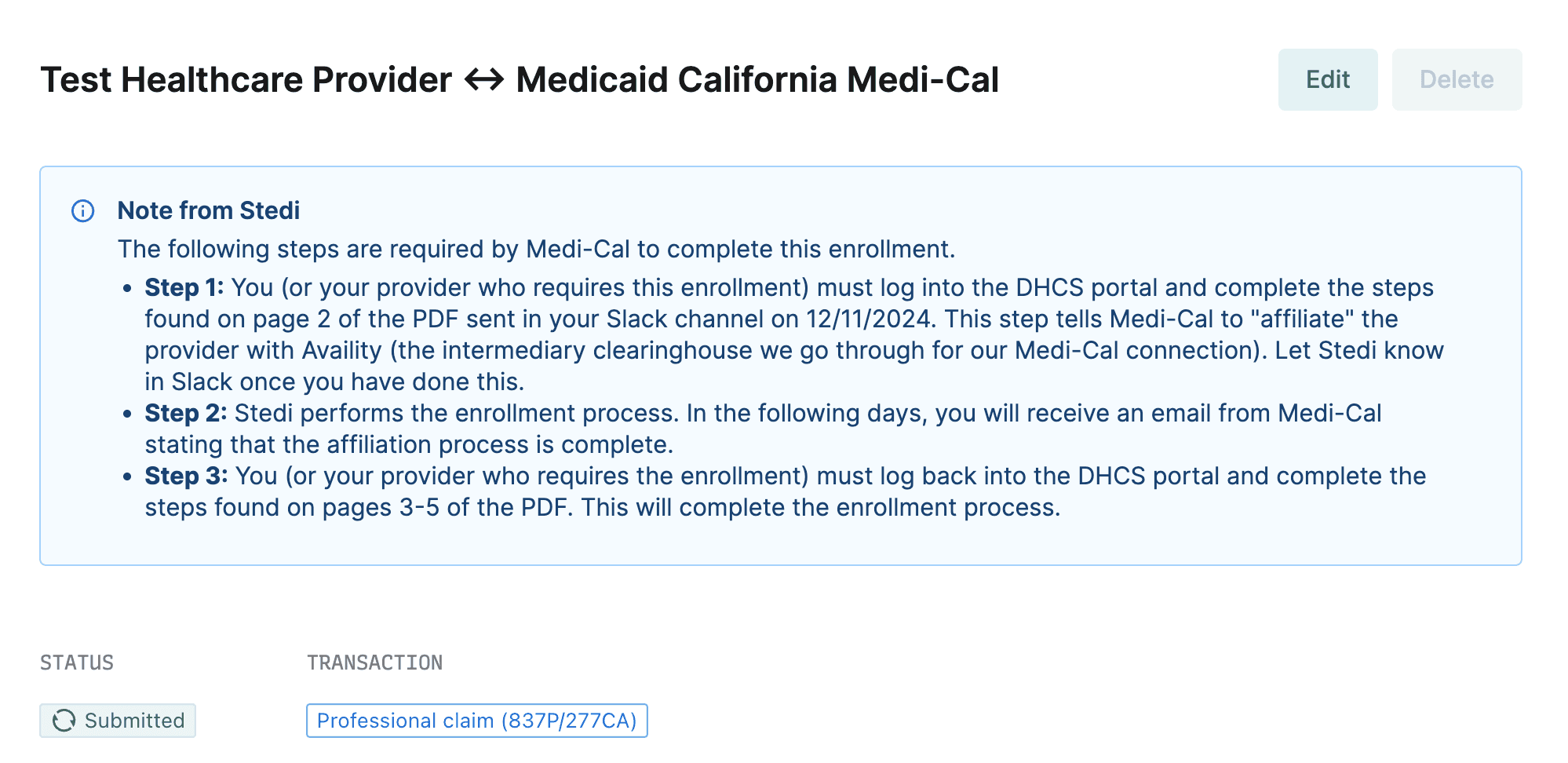
You can also retrieve this information through the GET Enrollment endpoint. Notes from Stedi about the next steps are available in the reason property.
{
"createdAt": "2024-12-11T22:39:16.772Z",
"id": "0193b7e0-6526-72a2-90a3-4e05dce4775a",
"payer": {
"id": "100065"
},
"primaryContact": {
"organizationName": "Test Healthcare Org",
"firstName": "",
"lastName": "",
"email": "test@testemail.com",
"phone": "4112334567",
"streetAddress1": "123 Some Street",
"streetAddress2": "",
"city": "Pittsburgh",
"zipCode": "12345",
"state": "PA"
},
"provider": {
"name": "Test Healthcare Provider",
"id": "0193b7db-528d-7723-9943-959b955ba103"
},
"reason": "The following steps are required by Medi-Cal to complete this enrollment.\n- **Step 1:** You (or your provider who requires this enrollment) must log into the DHCS portal and complete the steps found on page 2 of the PDF sent in your Slack channel on 12/11/2024. This step tells Medi-Cal to \"affiliate\" the provider with Availity (the intermediary clearinghouse we go through for our Medi-Cal connection). Let Stedi know in Slack once you have done this.\n- **Step 2:** Stedi performs the enrollment process. In the following days, you will receive an email from Medi-Cal stating that the affiliation process is complete.\n- **Step 3:** You (or your provider who requires the enrollment) must log back into the DHCS portal and complete the steps found on pages 3-5 of the PDF. This will complete the enrollment process.",
"status": "SUBMITTED",
"transactions": {
"professionalClaimSubmission": {
"enroll": true
}
},
"updatedAt": "2024-12-17T17:31:42.012Z",
"userEmail": "demos@stedi.com"
}Get started with Stedi today
Streamlined transaction enrollments are just one of the ways Stedi accelerates payer integration and offers a modern, developer-friendly alternative to traditional clearinghouses. You can search Stedi’s Payer Network to determine which payers require enrollment for the transaction types you need to process.
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows.
All payers require providers to complete an enrollment process before they can start receiving claim remittances (ERAs). Though less common, certain payers also require enrollment before allowing providers to submit transactions like claims and eligibility checks.
The typical enrollment process is highly manual and notoriously painful. There are no APIs or uniform standards, so every payer has different requirements. Forms, online portals, PDFs, wet signatures, and even fax machines can all be part of the process, causing significant frustration and slowing down the overall revenue cycle. After the enrollment is submitted, it’s a black box; days or weeks go by with no status updates, forcing providers to wait to submit claims, check patient eligibility, and receive information about payments. These issues compound for revenue cycle management companies that do hundreds or thousands of enrollments on behalf of many providers.
That’s why Stedi designed a new enrollment experience from the ground up. Through Stedi's user-friendly interface or modern API, developers and operations teams can now submit enrollments for specific transaction types in a streamlined flow – either one at a time or in large batches.
Once you submit an enrollment request, Stedi manages the entire process for you, including submitting the enrollment to the payer, following up as needed, and giving clear guidance for any additional steps that might be required. You can monitor the enrollment status throughout the process using the API or our searchable Enrollments dashboard.
Manage transaction enrollments through Stedi’s user-friendly app or APIs
You can submit and monitor all of your organization’s transaction enrollments from the Enrollments page in Stedi. For each enrollment request, Stedi displays the provider, status, payer, and transaction type. You can click any enrollment request to view its complete details, including any notes from Stedi regarding the next steps.
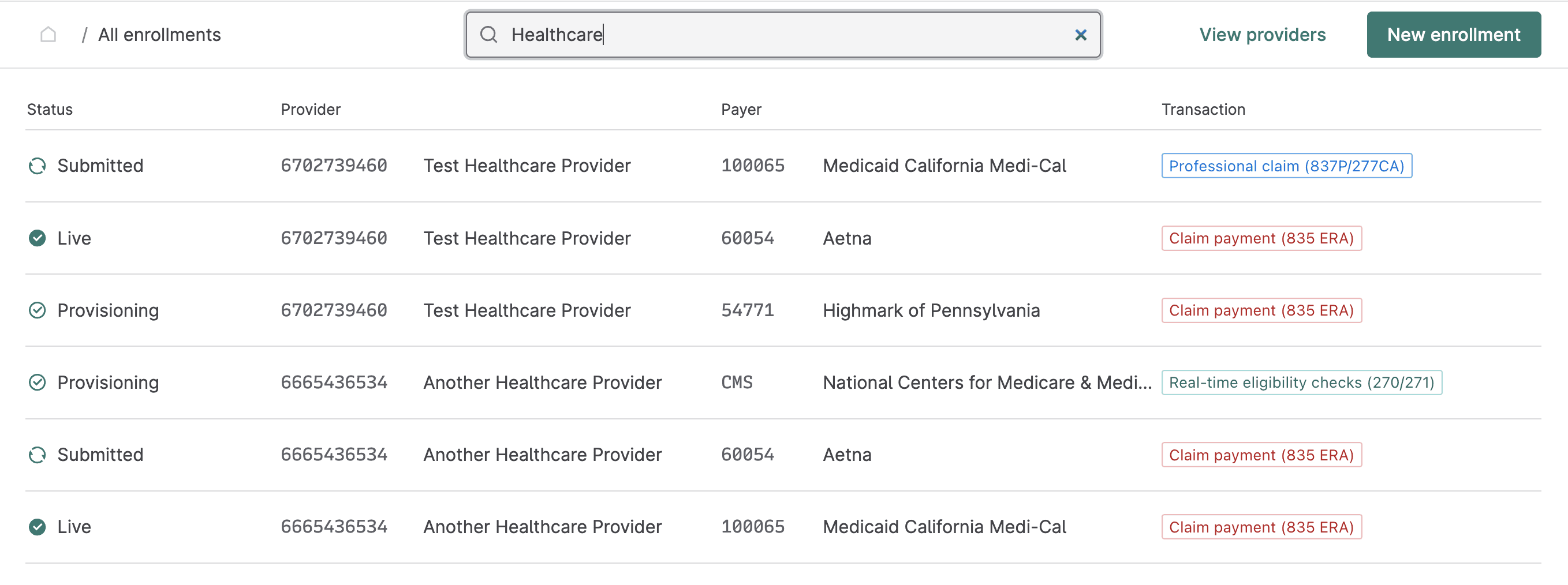
You can also manage the entire transaction enrollment process programmatically through Stedi’s Transaction Enrollment API. This approach is especially useful when you need to perform bulk enrollments for many providers at once, or when you want to embed enrollment capabilities into your own application. The following example request enrolls a provider for claim payments (835 ERAs) with UnitedHealthcare (Payer ID: 87726).
curl --request POST \
--url https://enrollments.us.stedi.com/2024-09-01/enrollments \
--header 'Authorization: <api-key>' \
--header 'Content-Type: application/json' \
--data '{
"transactions": {
"claimPayment": {
"enroll": true
}
},
"primaryContact": {
"firstName": "John",
"lastName": "Doe",
"email": "test@example.com",
"phone": "555-123-34354",
"streetAddress1": "123 Some Str.",
"city": "A City",
"state": "MD",
"zipCode": "20814"
},
"userEmail": "test@example.com",
"payer": {
"id": "87726"
},
"provider": {
"id": "db6665c5-7b97-4af9-8c68-a00a336c2998"
}
}'Streamlined processing
Transaction enrollment requests you submit manually and programmatically follow the same streamlined process:
Add provider: You add a new provider record with the information required for enrollment, including the provider's name, tax ID, NPI, and contact information.
Submit transaction enrollment requests: You submit requests to enroll the provider with required payers, one for each transaction type. For example, you’d submit three separate requests to enroll a provider for 837P (professional) claims, 270 real-time eligibility checks, and 835 ERAs (claim payments). You can save requests in
DRAFTstatus until you're ready to submit them to Stedi. Once you submit an enrollment request, its status is set toSUBMITTED, and it enters Stedi’s queue for processing.Provisioning: Stedi begins the enrollment process with the payer and sets the enrollment request status to
PROVISIONING. Our team leaves clear instructions about what to do next, if required, and provides hands-on help as needed with additional steps.Enrollment is Live: Once the enrollment is approved, the enrollment request status is set to
LIVE, and the provider can start exchanging the enrolled transactions with the payer.
Clear status updates and expert guidance
Our customer success team knows the nuances of each payer’s enrollment requirements and breaks them down into clear, actionable steps. In addition to updating your enrollment request with any action items required for your team, we also reach out to you in your dedicated Slack channel with resources and to answer any follow-up questions.
The following example shows an enrollment request for Medicaid California Medi-Cal that requires additional steps for the provider. In Step 1, customer support notes that they dropped the required PDF in Slack for easy access.
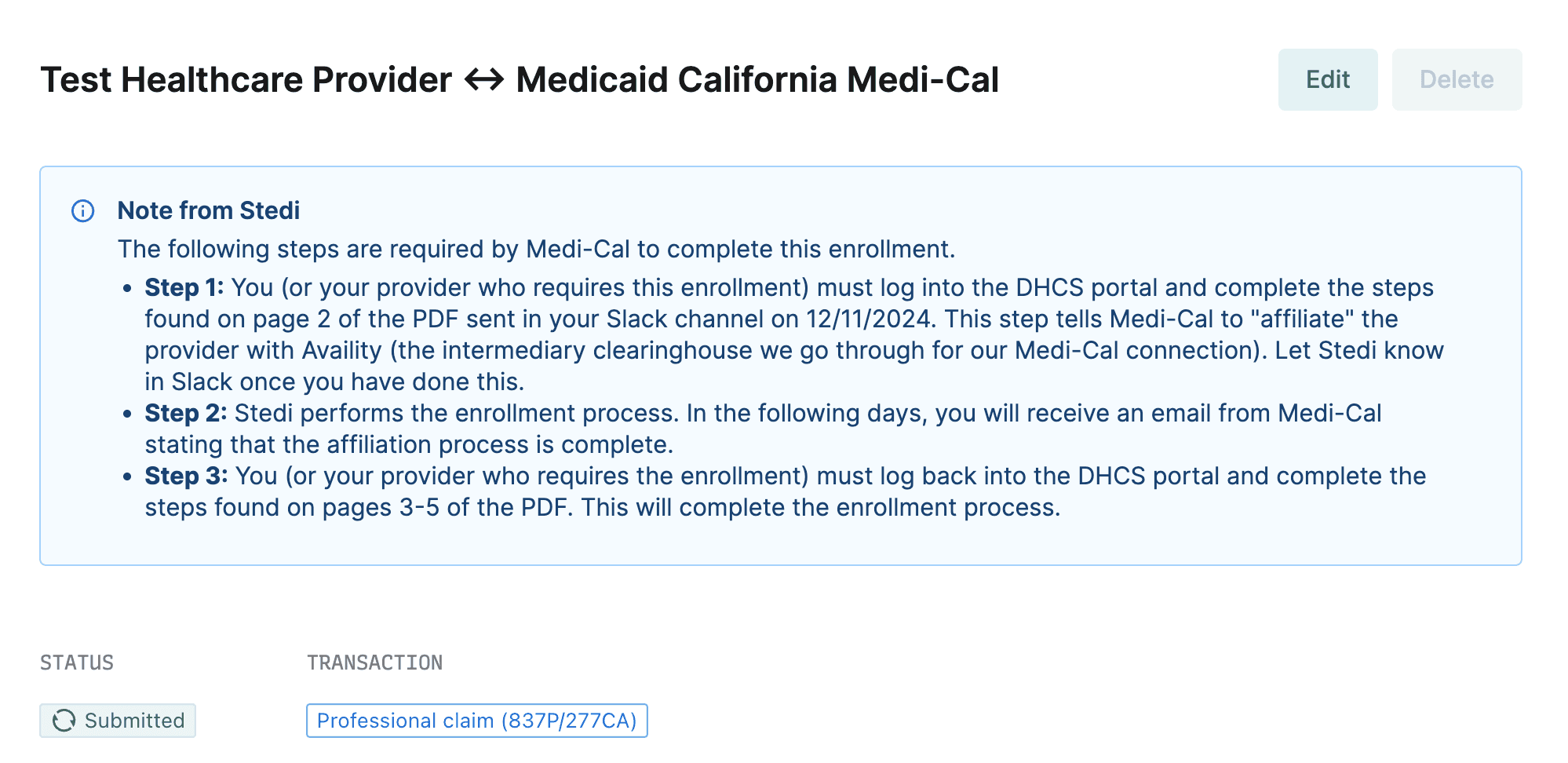
You can also retrieve this information through the GET Enrollment endpoint. Notes from Stedi about the next steps are available in the reason property.
{
"createdAt": "2024-12-11T22:39:16.772Z",
"id": "0193b7e0-6526-72a2-90a3-4e05dce4775a",
"payer": {
"id": "100065"
},
"primaryContact": {
"organizationName": "Test Healthcare Org",
"firstName": "",
"lastName": "",
"email": "test@testemail.com",
"phone": "4112334567",
"streetAddress1": "123 Some Street",
"streetAddress2": "",
"city": "Pittsburgh",
"zipCode": "12345",
"state": "PA"
},
"provider": {
"name": "Test Healthcare Provider",
"id": "0193b7db-528d-7723-9943-959b955ba103"
},
"reason": "The following steps are required by Medi-Cal to complete this enrollment.\n- **Step 1:** You (or your provider who requires this enrollment) must log into the DHCS portal and complete the steps found on page 2 of the PDF sent in your Slack channel on 12/11/2024. This step tells Medi-Cal to \"affiliate\" the provider with Availity (the intermediary clearinghouse we go through for our Medi-Cal connection). Let Stedi know in Slack once you have done this.\n- **Step 2:** Stedi performs the enrollment process. In the following days, you will receive an email from Medi-Cal stating that the affiliation process is complete.\n- **Step 3:** You (or your provider who requires the enrollment) must log back into the DHCS portal and complete the steps found on pages 3-5 of the PDF. This will complete the enrollment process.",
"status": "SUBMITTED",
"transactions": {
"professionalClaimSubmission": {
"enroll": true
}
},
"updatedAt": "2024-12-17T17:31:42.012Z",
"userEmail": "demos@stedi.com"
}Get started with Stedi today
Streamlined transaction enrollments are just one of the ways Stedi accelerates payer integration and offers a modern, developer-friendly alternative to traditional clearinghouses. You can search Stedi’s Payer Network to determine which payers require enrollment for the transaction types you need to process.
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows.
All payers require providers to complete an enrollment process before they can start receiving claim remittances (ERAs). Though less common, certain payers also require enrollment before allowing providers to submit transactions like claims and eligibility checks.
The typical enrollment process is highly manual and notoriously painful. There are no APIs or uniform standards, so every payer has different requirements. Forms, online portals, PDFs, wet signatures, and even fax machines can all be part of the process, causing significant frustration and slowing down the overall revenue cycle. After the enrollment is submitted, it’s a black box; days or weeks go by with no status updates, forcing providers to wait to submit claims, check patient eligibility, and receive information about payments. These issues compound for revenue cycle management companies that do hundreds or thousands of enrollments on behalf of many providers.
That’s why Stedi designed a new enrollment experience from the ground up. Through Stedi's user-friendly interface or modern API, developers and operations teams can now submit enrollments for specific transaction types in a streamlined flow – either one at a time or in large batches.
Once you submit an enrollment request, Stedi manages the entire process for you, including submitting the enrollment to the payer, following up as needed, and giving clear guidance for any additional steps that might be required. You can monitor the enrollment status throughout the process using the API or our searchable Enrollments dashboard.
Manage transaction enrollments through Stedi’s user-friendly app or APIs
You can submit and monitor all of your organization’s transaction enrollments from the Enrollments page in Stedi. For each enrollment request, Stedi displays the provider, status, payer, and transaction type. You can click any enrollment request to view its complete details, including any notes from Stedi regarding the next steps.
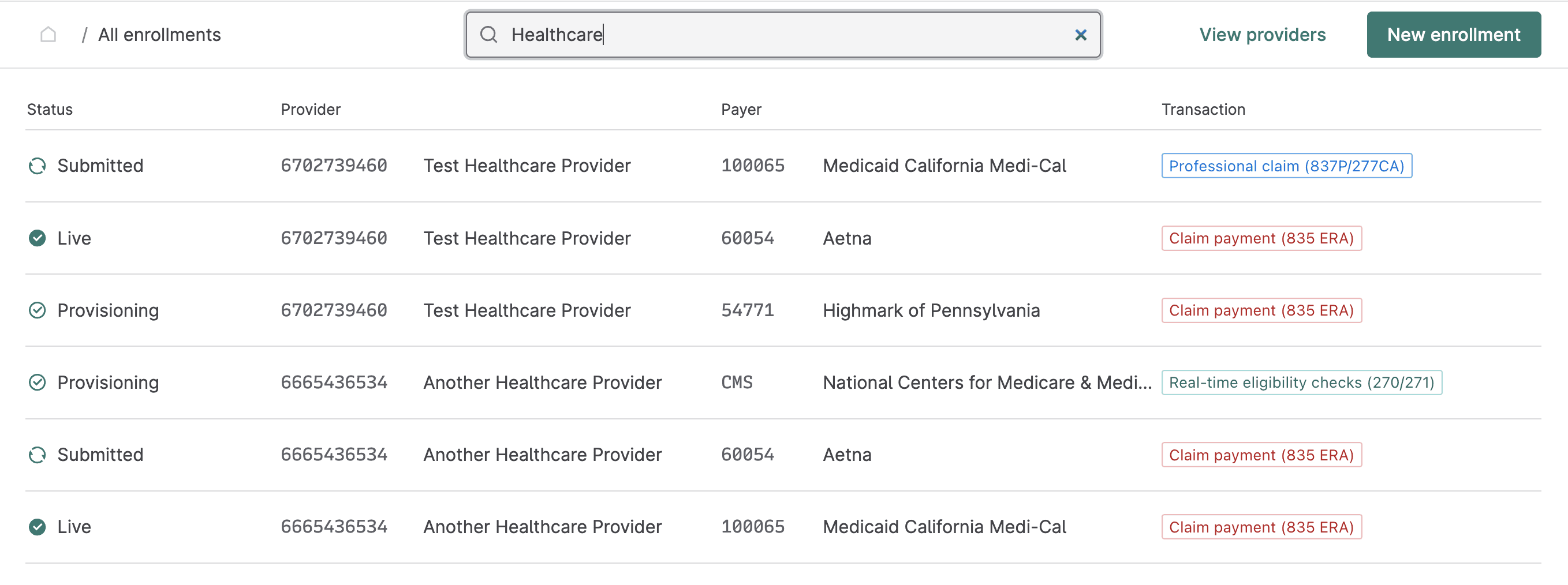
You can also manage the entire transaction enrollment process programmatically through Stedi’s Transaction Enrollment API. This approach is especially useful when you need to perform bulk enrollments for many providers at once, or when you want to embed enrollment capabilities into your own application. The following example request enrolls a provider for claim payments (835 ERAs) with UnitedHealthcare (Payer ID: 87726).
curl --request POST \
--url https://enrollments.us.stedi.com/2024-09-01/enrollments \
--header 'Authorization: <api-key>' \
--header 'Content-Type: application/json' \
--data '{
"transactions": {
"claimPayment": {
"enroll": true
}
},
"primaryContact": {
"firstName": "John",
"lastName": "Doe",
"email": "test@example.com",
"phone": "555-123-34354",
"streetAddress1": "123 Some Str.",
"city": "A City",
"state": "MD",
"zipCode": "20814"
},
"userEmail": "test@example.com",
"payer": {
"id": "87726"
},
"provider": {
"id": "db6665c5-7b97-4af9-8c68-a00a336c2998"
}
}'Streamlined processing
Transaction enrollment requests you submit manually and programmatically follow the same streamlined process:
Add provider: You add a new provider record with the information required for enrollment, including the provider's name, tax ID, NPI, and contact information.
Submit transaction enrollment requests: You submit requests to enroll the provider with required payers, one for each transaction type. For example, you’d submit three separate requests to enroll a provider for 837P (professional) claims, 270 real-time eligibility checks, and 835 ERAs (claim payments). You can save requests in
DRAFTstatus until you're ready to submit them to Stedi. Once you submit an enrollment request, its status is set toSUBMITTED, and it enters Stedi’s queue for processing.Provisioning: Stedi begins the enrollment process with the payer and sets the enrollment request status to
PROVISIONING. Our team leaves clear instructions about what to do next, if required, and provides hands-on help as needed with additional steps.Enrollment is Live: Once the enrollment is approved, the enrollment request status is set to
LIVE, and the provider can start exchanging the enrolled transactions with the payer.
Clear status updates and expert guidance
Our customer success team knows the nuances of each payer’s enrollment requirements and breaks them down into clear, actionable steps. In addition to updating your enrollment request with any action items required for your team, we also reach out to you in your dedicated Slack channel with resources and to answer any follow-up questions.
The following example shows an enrollment request for Medicaid California Medi-Cal that requires additional steps for the provider. In Step 1, customer support notes that they dropped the required PDF in Slack for easy access.
You can also retrieve this information through the GET Enrollment endpoint. Notes from Stedi about the next steps are available in the reason property.
{
"createdAt": "2024-12-11T22:39:16.772Z",
"id": "0193b7e0-6526-72a2-90a3-4e05dce4775a",
"payer": {
"id": "100065"
},
"primaryContact": {
"organizationName": "Test Healthcare Org",
"firstName": "",
"lastName": "",
"email": "test@testemail.com",
"phone": "4112334567",
"streetAddress1": "123 Some Street",
"streetAddress2": "",
"city": "Pittsburgh",
"zipCode": "12345",
"state": "PA"
},
"provider": {
"name": "Test Healthcare Provider",
"id": "0193b7db-528d-7723-9943-959b955ba103"
},
"reason": "The following steps are required by Medi-Cal to complete this enrollment.\n- **Step 1:** You (or your provider who requires this enrollment) must log into the DHCS portal and complete the steps found on page 2 of the PDF sent in your Slack channel on 12/11/2024. This step tells Medi-Cal to \"affiliate\" the provider with Availity (the intermediary clearinghouse we go through for our Medi-Cal connection). Let Stedi know in Slack once you have done this.\n- **Step 2:** Stedi performs the enrollment process. In the following days, you will receive an email from Medi-Cal stating that the affiliation process is complete.\n- **Step 3:** You (or your provider who requires the enrollment) must log back into the DHCS portal and complete the steps found on pages 3-5 of the PDF. This will complete the enrollment process.",
"status": "SUBMITTED",
"transactions": {
"professionalClaimSubmission": {
"enroll": true
}
},
"updatedAt": "2024-12-17T17:31:42.012Z",
"userEmail": "demos@stedi.com"
}Get started with Stedi today
Streamlined transaction enrollments are just one of the ways Stedi accelerates payer integration and offers a modern, developer-friendly alternative to traditional clearinghouses. You can search Stedi’s Payer Network to determine which payers require enrollment for the transaction types you need to process.
Contact us to speak to the team and learn how Stedi can help you automate and simplify your eligibility and claims workflows.
Share
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.