Institutional Claims API is Generally Available
Nov 20, 2024
Products
We’re excited to announce that our Institutional Claims API is now Generally Available.
Institutional claims are how hospitals, nursing homes, and other healthcare facilities bill insurers for services, such as inpatient care, diagnostics, and therapies. Our new Institutional Claims API allows you to automate this process and streamline the claims lifecycle for healthcare providers.
You can use the new API to submit 837I Institutional Claims to thousands of payers using Stedi’s developer-friendly JSON format. Once submitted, you can programmatically check the claim status in real time and retrieve 277 claim acknowledgments and 835 electronic remittance advice (ERA) from payers through the Stedi clearinghouse.
Submit institutional claims to thousands of payers
Call the Institutional Claims endpoint with a JSON payload. Stedi first validates your request against the 837I specification to ensure it’s compliant, reducing payer rejections down the line. Then, Stedi translates your request to the X12 837 EDI format and sends it to the payer. Finally, Stedi returns a response containing information about the claim you submitted and whether the submission was successful.
You can also send test claims to Stedi’s QA clearinghouse by setting the usageIndicator to T, as shown in the following example. This helps you quickly test and debug your end-to-end claims processing pipeline.
curl --request POST \ --url https://healthcare.us.stedi.com/2024-04-01/change/medicalnetwork/institutionalclaims/v1/submission \ --header 'Authorization: <api-key>' \ --header 'Content-Type: application/json' \ --data '{ "usageIndicator": "T", "tradingPartnerName": "UnitedHealthcare", "tradingPartnerServiceId": "87726", "controlNumber": "123456789", "submitter": { "organizationName": "Test Facility", "contactInformation": { "name": "Test Facility", "phoneNumber": "2225551234" }, "taxId": "123456789" }, "receiver": { "organizationName": "UnitedHealthcare" }, "subscriber": { "memberId": "98765", "paymentResponsibilityLevelCode": "P", "firstName": "JANE", "lastName": "DOE", "groupNumber": "67890" }, "claimInformation": { "claimFilingCode": "ZZ", "patientControlNumber": "00001111222233334444", "claimChargeAmount": "500.00", "placeOfServiceCode": "11", "claimFrequencyCode": "0", "planParticipationCode": "C", "benefitsAssignmentCertificationIndicator": "Y", "releaseInformationCode": "Y", "principalDiagnosis": { "qualifierCode": "ABK", "principalDiagnosisCode": "R45851" }, "serviceLines": [ { "assignedNumber": "0", "serviceDate": "20241015", "serviceDateEnd": "20241015", "lineItemControlNumber": "111222333", "institutionalService": { "serviceLineRevenueCode": "90", "lineItemChargeAmount": "500.00", "measurementUnit": "UN", "serviceUnitCount": "1", "procedureIdentifier": "HC", "procedureCode": "H0001" } } ], "claimCodeInformation": { "admissionTypeCode": "3", "admissionSourceCode": "9", "patientStatusCode": "30" }, "claimDateInformation": { "admissionDateAndHour": "202409091000", "statementBeginDate": "20241015", "statementEndDate": "20241015" } }, "providers": [ { "providerType": "BillingProvider", "npi": "0123456789", "employerId": "123456789", "organizationName": "Test Facility", "address": { "address1": "123 Mulberry Street", "city": "Seattle", "state": "WA", "postalCode": "111135272" }, "contactInformation": { "name": "Test Facility", "phoneNumber": "2065551234" } }, { "providerType": "AttendingProvider", "npi": "1234567890", "firstName": "Doctor", "lastName": "Provider", "contactInformation": { "name": "name" } } ] }'
Retrieve 277 acknowledgments and 835 ERAs programmatically
After you submit an institutional claim, you may receive asynchronous 277CA and 835 ERA responses from the payer. The 277CA indicates whether the claim was accepted or rejected and (if relevant) the reasons for rejection. The 835 ERA, also known as a claim remittance, contains details about payments for specific services and explanations for any adjustments or denials.
You can either poll Stedi for processed 277CAs and 835 ERAs or set up webhooks that automatically send events for processed responses to your endpoint. Then, you can use the following APIs to retrieve them from Stedi in JSON format:
Get 277CA Report: Retrieve 277CA responses
Get 835 ERA Report: Retrieve 835 ERA responses
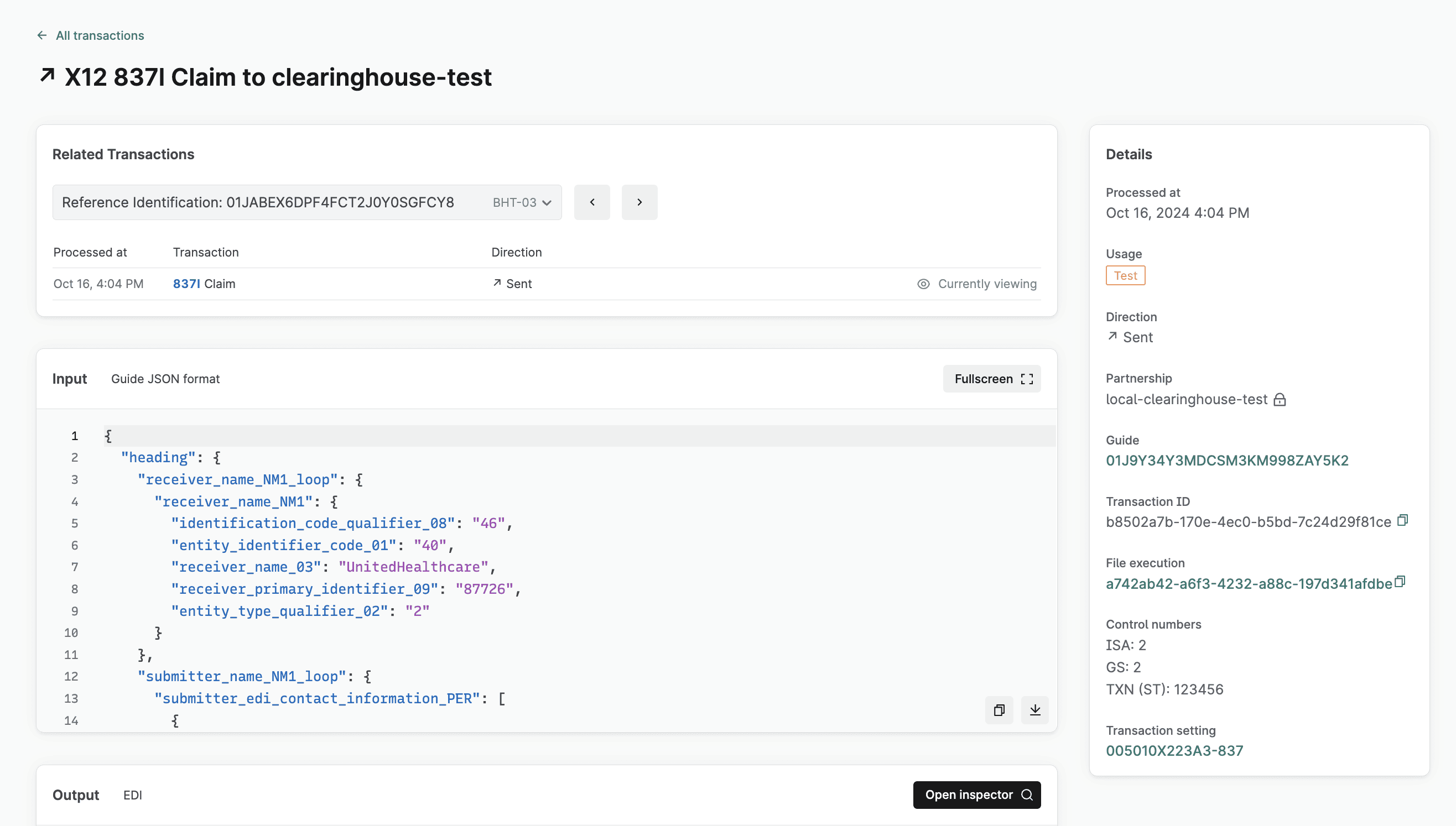
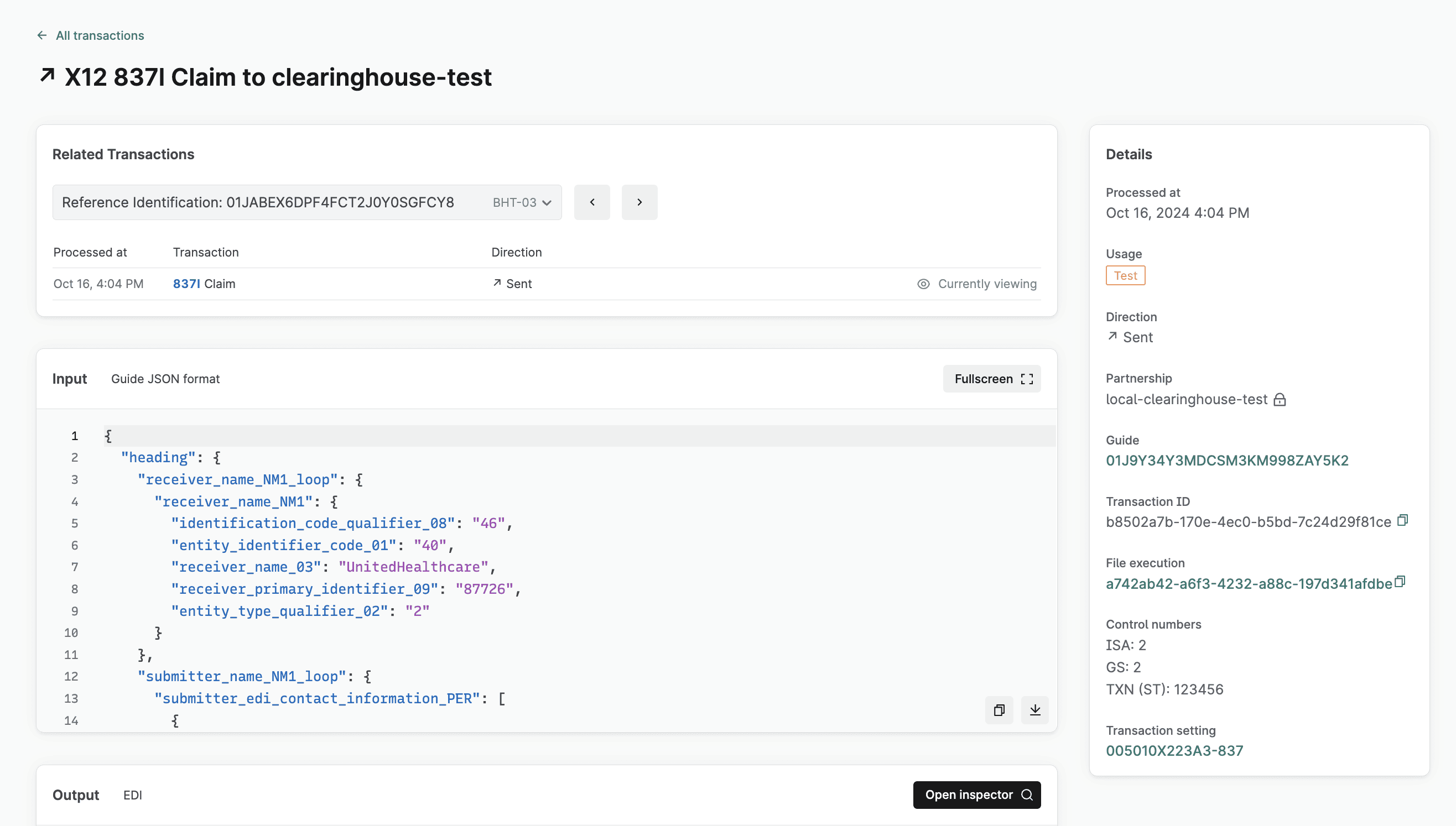
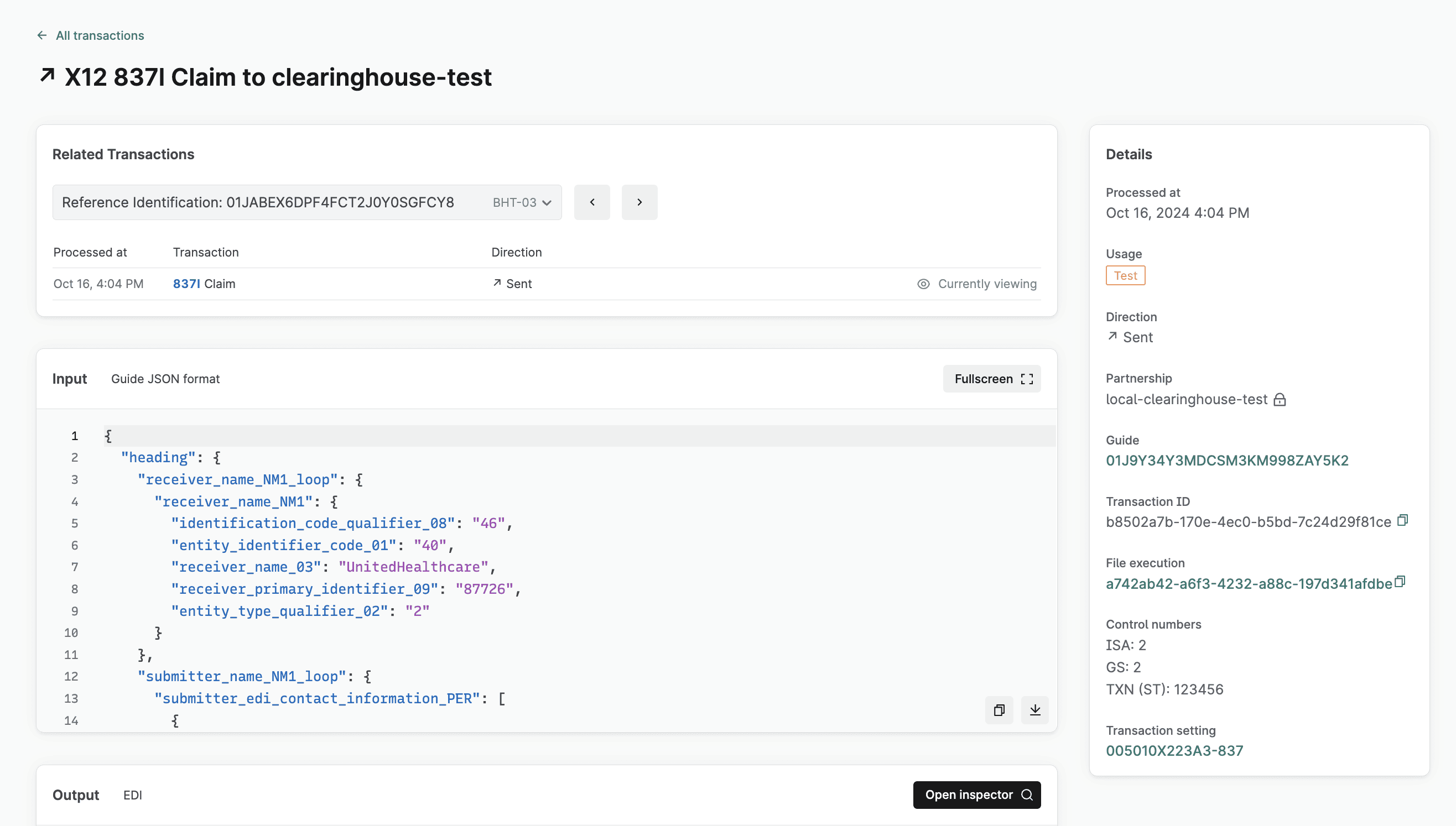
Track claims and responses in the Stedi app
You can view a list of every claim you submit through the Stedi clearinghouse and all associated responses on the Transactions page of the Stedi app. Click any transaction to review its details, including the full request and response payload.
Start processing claims with Stedi
With the Institutional Claims API, you can start automating your claim submission process today. Contact us to learn more and speak to the team.
We’re excited to announce that our Institutional Claims API is now Generally Available.
Institutional claims are how hospitals, nursing homes, and other healthcare facilities bill insurers for services, such as inpatient care, diagnostics, and therapies. Our new Institutional Claims API allows you to automate this process and streamline the claims lifecycle for healthcare providers.
You can use the new API to submit 837I Institutional Claims to thousands of payers using Stedi’s developer-friendly JSON format. Once submitted, you can programmatically check the claim status in real time and retrieve 277 claim acknowledgments and 835 electronic remittance advice (ERA) from payers through the Stedi clearinghouse.
Submit institutional claims to thousands of payers
Call the Institutional Claims endpoint with a JSON payload. Stedi first validates your request against the 837I specification to ensure it’s compliant, reducing payer rejections down the line. Then, Stedi translates your request to the X12 837 EDI format and sends it to the payer. Finally, Stedi returns a response containing information about the claim you submitted and whether the submission was successful.
You can also send test claims to Stedi’s QA clearinghouse by setting the usageIndicator to T, as shown in the following example. This helps you quickly test and debug your end-to-end claims processing pipeline.
curl --request POST \ --url https://healthcare.us.stedi.com/2024-04-01/change/medicalnetwork/institutionalclaims/v1/submission \ --header 'Authorization: <api-key>' \ --header 'Content-Type: application/json' \ --data '{ "usageIndicator": "T", "tradingPartnerName": "UnitedHealthcare", "tradingPartnerServiceId": "87726", "controlNumber": "123456789", "submitter": { "organizationName": "Test Facility", "contactInformation": { "name": "Test Facility", "phoneNumber": "2225551234" }, "taxId": "123456789" }, "receiver": { "organizationName": "UnitedHealthcare" }, "subscriber": { "memberId": "98765", "paymentResponsibilityLevelCode": "P", "firstName": "JANE", "lastName": "DOE", "groupNumber": "67890" }, "claimInformation": { "claimFilingCode": "ZZ", "patientControlNumber": "00001111222233334444", "claimChargeAmount": "500.00", "placeOfServiceCode": "11", "claimFrequencyCode": "0", "planParticipationCode": "C", "benefitsAssignmentCertificationIndicator": "Y", "releaseInformationCode": "Y", "principalDiagnosis": { "qualifierCode": "ABK", "principalDiagnosisCode": "R45851" }, "serviceLines": [ { "assignedNumber": "0", "serviceDate": "20241015", "serviceDateEnd": "20241015", "lineItemControlNumber": "111222333", "institutionalService": { "serviceLineRevenueCode": "90", "lineItemChargeAmount": "500.00", "measurementUnit": "UN", "serviceUnitCount": "1", "procedureIdentifier": "HC", "procedureCode": "H0001" } } ], "claimCodeInformation": { "admissionTypeCode": "3", "admissionSourceCode": "9", "patientStatusCode": "30" }, "claimDateInformation": { "admissionDateAndHour": "202409091000", "statementBeginDate": "20241015", "statementEndDate": "20241015" } }, "providers": [ { "providerType": "BillingProvider", "npi": "0123456789", "employerId": "123456789", "organizationName": "Test Facility", "address": { "address1": "123 Mulberry Street", "city": "Seattle", "state": "WA", "postalCode": "111135272" }, "contactInformation": { "name": "Test Facility", "phoneNumber": "2065551234" } }, { "providerType": "AttendingProvider", "npi": "1234567890", "firstName": "Doctor", "lastName": "Provider", "contactInformation": { "name": "name" } } ] }'
Retrieve 277 acknowledgments and 835 ERAs programmatically
After you submit an institutional claim, you may receive asynchronous 277CA and 835 ERA responses from the payer. The 277CA indicates whether the claim was accepted or rejected and (if relevant) the reasons for rejection. The 835 ERA, also known as a claim remittance, contains details about payments for specific services and explanations for any adjustments or denials.
You can either poll Stedi for processed 277CAs and 835 ERAs or set up webhooks that automatically send events for processed responses to your endpoint. Then, you can use the following APIs to retrieve them from Stedi in JSON format:
Get 277CA Report: Retrieve 277CA responses
Get 835 ERA Report: Retrieve 835 ERA responses
Track claims and responses in the Stedi app
You can view a list of every claim you submit through the Stedi clearinghouse and all associated responses on the Transactions page of the Stedi app. Click any transaction to review its details, including the full request and response payload.
Start processing claims with Stedi
With the Institutional Claims API, you can start automating your claim submission process today. Contact us to learn more and speak to the team.
We’re excited to announce that our Institutional Claims API is now Generally Available.
Institutional claims are how hospitals, nursing homes, and other healthcare facilities bill insurers for services, such as inpatient care, diagnostics, and therapies. Our new Institutional Claims API allows you to automate this process and streamline the claims lifecycle for healthcare providers.
You can use the new API to submit 837I Institutional Claims to thousands of payers using Stedi’s developer-friendly JSON format. Once submitted, you can programmatically check the claim status in real time and retrieve 277 claim acknowledgments and 835 electronic remittance advice (ERA) from payers through the Stedi clearinghouse.
Submit institutional claims to thousands of payers
Call the Institutional Claims endpoint with a JSON payload. Stedi first validates your request against the 837I specification to ensure it’s compliant, reducing payer rejections down the line. Then, Stedi translates your request to the X12 837 EDI format and sends it to the payer. Finally, Stedi returns a response containing information about the claim you submitted and whether the submission was successful.
You can also send test claims to Stedi’s QA clearinghouse by setting the usageIndicator to T, as shown in the following example. This helps you quickly test and debug your end-to-end claims processing pipeline.
curl --request POST \ --url https://healthcare.us.stedi.com/2024-04-01/change/medicalnetwork/institutionalclaims/v1/submission \ --header 'Authorization: <api-key>' \ --header 'Content-Type: application/json' \ --data '{ "usageIndicator": "T", "tradingPartnerName": "UnitedHealthcare", "tradingPartnerServiceId": "87726", "controlNumber": "123456789", "submitter": { "organizationName": "Test Facility", "contactInformation": { "name": "Test Facility", "phoneNumber": "2225551234" }, "taxId": "123456789" }, "receiver": { "organizationName": "UnitedHealthcare" }, "subscriber": { "memberId": "98765", "paymentResponsibilityLevelCode": "P", "firstName": "JANE", "lastName": "DOE", "groupNumber": "67890" }, "claimInformation": { "claimFilingCode": "ZZ", "patientControlNumber": "00001111222233334444", "claimChargeAmount": "500.00", "placeOfServiceCode": "11", "claimFrequencyCode": "0", "planParticipationCode": "C", "benefitsAssignmentCertificationIndicator": "Y", "releaseInformationCode": "Y", "principalDiagnosis": { "qualifierCode": "ABK", "principalDiagnosisCode": "R45851" }, "serviceLines": [ { "assignedNumber": "0", "serviceDate": "20241015", "serviceDateEnd": "20241015", "lineItemControlNumber": "111222333", "institutionalService": { "serviceLineRevenueCode": "90", "lineItemChargeAmount": "500.00", "measurementUnit": "UN", "serviceUnitCount": "1", "procedureIdentifier": "HC", "procedureCode": "H0001" } } ], "claimCodeInformation": { "admissionTypeCode": "3", "admissionSourceCode": "9", "patientStatusCode": "30" }, "claimDateInformation": { "admissionDateAndHour": "202409091000", "statementBeginDate": "20241015", "statementEndDate": "20241015" } }, "providers": [ { "providerType": "BillingProvider", "npi": "0123456789", "employerId": "123456789", "organizationName": "Test Facility", "address": { "address1": "123 Mulberry Street", "city": "Seattle", "state": "WA", "postalCode": "111135272" }, "contactInformation": { "name": "Test Facility", "phoneNumber": "2065551234" } }, { "providerType": "AttendingProvider", "npi": "1234567890", "firstName": "Doctor", "lastName": "Provider", "contactInformation": { "name": "name" } } ] }'
Retrieve 277 acknowledgments and 835 ERAs programmatically
After you submit an institutional claim, you may receive asynchronous 277CA and 835 ERA responses from the payer. The 277CA indicates whether the claim was accepted or rejected and (if relevant) the reasons for rejection. The 835 ERA, also known as a claim remittance, contains details about payments for specific services and explanations for any adjustments or denials.
You can either poll Stedi for processed 277CAs and 835 ERAs or set up webhooks that automatically send events for processed responses to your endpoint. Then, you can use the following APIs to retrieve them from Stedi in JSON format:
Get 277CA Report: Retrieve 277CA responses
Get 835 ERA Report: Retrieve 835 ERA responses
Track claims and responses in the Stedi app
You can view a list of every claim you submit through the Stedi clearinghouse and all associated responses on the Transactions page of the Stedi app. Click any transaction to review its details, including the full request and response payload.
Start processing claims with Stedi
With the Institutional Claims API, you can start automating your claim submission process today. Contact us to learn more and speak to the team.
Share
Get started with Stedi
Get started with Stedi
Automate healthcare transactions with developer-friendly APIs that support thousands of payers. Contact us to learn more and speak to the team.
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Get updates on what’s new at Stedi
Developers
Resources
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.
Developers
Resources
Get updates on what’s new at Stedi
Backed by
Stedi is a registered trademark of Stedi, Inc. All names, logos, and brands of third parties listed on our site are trademarks of their respective owners (including “X12”, which is a trademark of X12 Incorporated). Stedi, Inc. and its products and services are not endorsed by, sponsored by, or affiliated with these third parties. Our use of these names, logos, and brands is for identification purposes only, and does not imply any such endorsement, sponsorship, or affiliation.